Foot Massage Techniques for Heel Pain
 Not only does massage feel great–it’s a great way to temporarily relieve heel pain from plantar fasciitis.
With a little know-how and a few easy techniques, you can learn to to do self massage on your own feet, or with a partner. All you’ll need to get started is a little baby oil or other lubricant and the information in this blog post!
Not only does massage feel great–it’s a great way to temporarily relieve heel pain from plantar fasciitis.
With a little know-how and a few easy techniques, you can learn to to do self massage on your own feet, or with a partner. All you’ll need to get started is a little baby oil or other lubricant and the information in this blog post!
The Benefits of Self Massage for Plantar Fasciitis
Your natural response to many types of pain is to rub the area. Why? Because we instinctively know that massage can help relieve aches and pains. Heel pain from plantar fasciitis is no exception. By rubbing the heel, arch, and surrounding areas, you can stimulate blood flow to the area, improve circulation, break down adhesions and scarring, temporarily diminish the pain signals from nerve endings, and stretch and loosen tight muscles and tendons that contribute to plantar fasciitis.
Supplies You’ll Need for a Heel Pain Massage
All you’ll need to get started massaging your feet and heels is a comfortable place to sit that allows you to reach your feet easily. You’ll also need baby oil or another lubricant that can glide easily over the surface of your skin. This lubricant will help you massage in a smooth, controlled motion. You’ll only need a pea-sized amount for one foot. Too much will turn into a gloppy mess and may cause too much slipping and sliding. You’ll also want to keep a few paper towels handy, so you don’t have to walk on slippery, oily feet. If you’re doing self massage, you may consider using an aide like a frozen water bottle, rolling pin, golf ball, or special Massage Ball. These tools can help you target pressure more effectively and get a more even massage than is possible with your own hands.Solo Foot Massage Techniques
There are several simple, effective techniques you can use to massage your own feet at home, or on a break at work. As you massage, apply as much pressure as you comfortably can–but never to the point of pain. Before you dive into a massage, spend a couple of minutes warming up the oil and rubbing the entire surface of your foot using smooth movements.Massaging with your hands:
Focus on the base of your heel where your plantar fascia ligament meets the heel bone, and massage in a circular motion with your thumbs in smooth, even movements. You can also apply pressure and massage lengthwise along the plantar fascia ligament from the ball of your foot down to the base of the heel bone.Using a golf ball, tennis ball, or water bottle
Most of us have one of these handy tools lying around the house. To massage your feet with a ball or water bottle, sit in a chair with your feet facing forward. Next, roll your foot from the ball of your foot to the heel, applying as much pressure as you can. You can also try using a frozen water bottle, for the added benefit of soothing cold and to reduce inflammation!Using a Massage Ball
 A Massage Ball is similar to the tools mentioned above that help with self massage, with the added benefits of being easy to clean, and easy to slip into a bag or purse. A Massage Ball also has a bit of give to it that will allow you to easily apply different levels of pressure while you roll it.
A Massage Ball is similar to the tools mentioned above that help with self massage, with the added benefits of being easy to clean, and easy to slip into a bag or purse. A Massage Ball also has a bit of give to it that will allow you to easily apply different levels of pressure while you roll it.
Foot Massage Techniques with a Partner
If you have a spouse, partner, or friend who is willing to massage your feet, there are a number of easy-to-learn techniques they can use. You’ll find that many are the same techniques used by professionals who specialize in sports medicine! Have your partner sit facing you, in a position that allows him or her to support your foot on a cushion or other surface while not actively massaging (feet and legs are heavy!).Knuckle or thumb massage:
 After warming up, have your partner use their knuckles or thumbs to move in small smooth circles along the bottom of your foot. Make sure to communicate about pressure level!
After warming up, have your partner use their knuckles or thumbs to move in small smooth circles along the bottom of your foot. Make sure to communicate about pressure level!
Top strokes with fingers:
While cupping your heel in the base of one hand, have your partner use the tips of their fingers to apply light pressure as they stroke the top and sides of your feet, forward and back. Remember, it’s helpful to massage areas that surround the heel and fascia too, since muscles and ligaments in the foot are interconnected!Deep-pressure hand massage:
Have your partner use the heel of their hand to apply steady pressure, moving from the ball of the foot to the heel, and back again.Rocking heel massage:
Lay on your back with your partner facing you. Have your partner use one hand to hold the upper part of your foot (the toes and the ball of your foot), while cupping your heel in their hand. Have your partner rock your heel gently from side to side, while massaging the heel with the thumb that is cupping it.Wringing massage:
Lie on your back with your partner facing you and one leg raised so that your knee and leg form a 90 degree angle. Have your partner place their hands facing opposite directions then apply gentle pressure and twist each hand, as if wringing out a wet washcloth. Have you partner move their hands over different parts of each foot, including ball, instep, and arch, while performing the same motion.Dorsiflexion stretch:
Have you partner hold your toes and ball of your foot with one hand while supporting your heel with the other. While gently pulling the toes and ball of your foot toward your shin bone (dorsiflexion), have your partner use their thumbs to apply gentle pressure up and down your arch. Stay in good communication during this stretch, since it can be painful if too much pressure is applied.Tips for Successful Plantar Fasciitis Massage
While massage isn’t a permanent treatment and will relieve pain only temporarily, it is more effective than simply resting your heel! Massage can be performed any time of the day, while you are watching TV, first thing in the morning, or during a break at work. No matter which massage techniques you choose to use, make sure to apply pressure that is firm but not painful. If massage is painful for you, try applying less pressure, or consider another pain relief method. When massaging with a partner, make sure you feel comfortable speaking up if the pressure is too great or if a particular motion is causing you pain instead of relieving it. In general, most massages should be performed for between 5-15 minutes at a time. As with any form of treatment, keep your doctors in the loop before starting a regimen of massage! Because any pain relief you may experience from heel pain massage is temporary, it’s also important to treat the underlying cause of your plantar fasciitis by wearing supportive footwear and orthotic inserts, maintaining a healthy weight, stretching your feet and legs, and resting as needed. |
|---|
What is Trigger Toe?
Trigger finger, also known as “stenosing tenosynovitis” is a condition that causes your finger to become “stuck” in a bent position. When forced to straighten, the appendage snaps into the new position rather than transitioning smoothly (like the trigger on a pistol).
Trigger finger is common in individuals whose jobs or recreational activities include a lot of gripping and repetitive fingerwork, and is caused by inflammation and swelling of the sheath that protects the tendons in your fingers.
Many disorders of the fingers are found in the toes, and vice versa. So, is there such a thing as trigger toe?
Can You Get Trigger Finger in Your Toes?
Short answer, yes!
That said, trigger toe is a relatively uncommon foot condition that typically affects only a small subset of people: mainly dancers who perform en pointe. Dancing en pointe puts pressure on the big toe, which can irritate and inflame the sheath protecting the tendon in the big toe.
What Causes Trigger Toe?
The tendon that ends in the big toe, the flexor hallucis longus, moves in and out through the calf and down the foot as you flex and move your feet and legs. Typically, this motion is smooth and seamless. However, through overuse and excessive strain (such as by placing the weight of the body on the toes constantly during dance), the sheath that houses this tendon can become tender, inflamed, and swollen.
When the tendon sheath swells, it becomes more difficult for the tendon to slide through smoothly, resulting in lockups and jerky transitions–or trigger-toe. Left untreated, trigger toe can cause damage and scarring to the FHL tendon.
Symptoms of Trigger Toe
While the symptoms of trigger toe are typically mild in the beginning, it’s important not to ignore them. Left untreated, trigger toe can cause permanent and irreversible damage. In the case of a professional dancer, this can mean the end of a career.
The first symptoms of trigger toe include mid discomfort in the big toe and brief lockups that easily release. However, as the condition worsens, it may become very difficult to dance en pointe, because of the sharp pain in the toe. Lockups will become worse as well, requiring a dancer to manually bend or straighten the toe that has become locked.
You may also notice stiffness in the big toe, especially in the morning, tenderness in the toe and foot, or a “clicking” sound as the toe locks in and out of different positions. Trigger toe can affect one or both big toes.
Treating and Preventing Trigger Toe
While the general population will likely never experience trigger toe, dancers and some athletes should stay vigilant to symptoms that could signify the condition and consult a doctor as soon as symptoms present themselves.
Allowing your feet proper rest during and between dance sessions, properly warming up the toes, feet, ankles, and calves with stretches before and after a workout, and icing can help keep your toes and feet healthy. NSAIDs can also be used to reduce swelling and inflammation. In very severe cases, your doctor may perform a surgery to release the FHL tendon.
While trigger toe is relatively uncommon, it’s very important to treat symptoms quickly if they arise–particularly if you are a dancer or athlete. Taking action to address the underlying problem and rest your toes properly will help avoid long-term damage and early retirement from a hobby or career you love.
Indoor Exercises You Can Do with Plantar Fasciitis
 Let’s face it: getting to the gym isn’t always the best option for exercise.
Let’s face it: getting to the gym isn’t always the best option for exercise.
Whether it’s financial restrictions, freezing rain, or just the struggle of getting out of the house, having a repertoire of good indoor exercise options is a smart way to keep your fitness and health goals on track.
Losing weight, strengthening muscles and ligaments that support your heel and arches, and enjoying the rush of endorphins and other health benefits that go hand in hand with exercise are all good reasons to continue your exercise routine at home, even when the gym or outdoor exercise aren’t options.
But what are the best indoor exercise programs and routines that you can do with plantar fasciitis?
(Hint: It’s not P90X!)
The Best Indoor Exercises for Plantar Fasciitis
When it comes to indoor exercise programs, Insanity and P90X are two of the most popular options out there. But with all those jumps, lunges, and sudden movements, both are much too high-impact for individuals who suffer from plantar fasciitis.
If you have heel pain from plantar fasciitis, you’ll want to avoid anything with lots of jumping, bouncing, running in place, lunges, or plyometrics.
And no matter which indoor exercise program you choose, you’ll want to choose high-quality, supportive footwear combined with orthotic inserts to support and realign arches.
Make sure to stretch before and after any kind of exercise to warm up and stretch your muscles and ligaments, and keep your doctor in the loop before you start any new exercise program.
Best Low-Impact Indoor Cardio Exercise Programs
Cardio is important for weight loss, heart health, and so many other health benefits that come from getting your heart rate up and your body moving.
While many types of cardio can be a big no-no for plantar fasciitis sufferers, including running and some types of sports, the following exercise programs are easy on your heels while giving you all the benefits of a great cardio workout:
HIIT Workouts
High Intensity Interval Training is a great way to get your cardio in at home. And don’t let the name fool you! High intensity doesn’t have to mean high impact. This type of workout alternates between bursts of activity and recovery periods to get your heart pumping. While there are many types of HIIT workouts to choose from, make sure to opt for a low-impact HIIT program (there’s a lot!)

Recommended: XTrain’s All Out Low Impact HIIT DVD (the only equipment needed is set of light hand weights)
Recommended: HASFit’s Low Impact Cardio HIIT (Many of these workouts are free and available online!)
Pi-Yo Aerobics
While many people associate aerobics with a lot of jumping and dancing, many exercise programs have been developed as low-impact alternatives to all the heavy footwork, by using elements from pilates and yoga combined with aerobics. Look for programs that skip running in place, jumping, and kicking.
Seated Cardio Exercises
Yes, it’s a thing! If standing is too painful with your plantar fasciitis and heel pain, there are many exercise programs that can be done for home, using only a chair. Stay seated the whole time, but get that blood pumping!
Recommended: SparkPeople’s Seated Cardio (Totally free!)
Low-Impact Indoor Strength Exercise Programs
Looking to tone your muscles and develop greater strength at home? You’re in good company. The following exercise programs will help strengthen and tone your core and key muscle groups, no special equipment required.
Pilates

Pilates is all about building endurance, flexibility, and muscles strength–with low impact moves. There’s no special equipment required, meaning it can be done at home in your living room! Routines are typically short, and often focused on a particular muscle group or section of the body.
Recommendation: FitnessBlender offers tons of free, low impact pilates routines that you can do at home
Tai Chi
Tai Chi, an Eastern discipline, can be a terrific option for strength training and muscle building. The fluid motions and very low impact exercise can be a great way to build and align muscles in the legs and feet, which support your arches.
Recommendation: Tai Chi Health offers a terrific program that lays out options for all ability levels, including a completely seated program.
Yoga or Pi-Yo
Yoga and Pi-Yo (a workout that combines moves from both yoga and pilates) are two of the best low-impact strength-training options for individuals with plantar fasciitis. Both styles of exercise focus on flexibility, strength in core muscle groups, and creating alignment throughout the body. Many of the moves will allow you to stay seated, or can be modified to take pressure off tender heels and feet.
Recommendation: Boho Beautiful offers some great, free yoga videos for beginners
Recommendation: BeachBody has excellent Pi-Yo DVD options with “no jumps, no weights”
What’s your favorite low-impact cardio or strength regimen? Share your recommendations in the comments below! Because no matter how you choose to stay active with plantar fasciitis, you should feel proud of your efforts to stay fit and healthy. Keep up the good work!
 |
|
|---|
Could Your Heel Pain Be Bursitis?
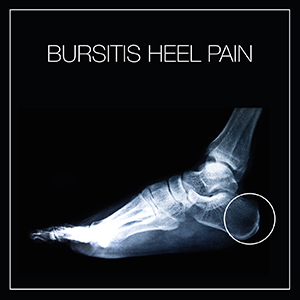 Is that pain and swelling in your heel and foot area plantar fasciitis? Or could it be another fairly common condition, known as bursitis?
Is that pain and swelling in your heel and foot area plantar fasciitis? Or could it be another fairly common condition, known as bursitis?
While the majority of cases involving heel pain turn out to be plantar fasciitis, numerous other conditions can cause heel pain. Knowing the difference between them can help you quickly identify and seek the proper treatment for your pain, allowing you to get back on your feet quickly and without complications.
What Is Bursitis?
Bursitis is an inflammatory condition that affects the bursae, or tiny fluid-filled sacs located near the joints in your body. Under normal conditions, these sacs help your joints move smoothly and play a role in protecting and cushioning different parts of the joint as you move, like tendons, ligaments, and muscles. Bursitis develops when these fluid-filled sacs become inflamed, swollen, and painful.
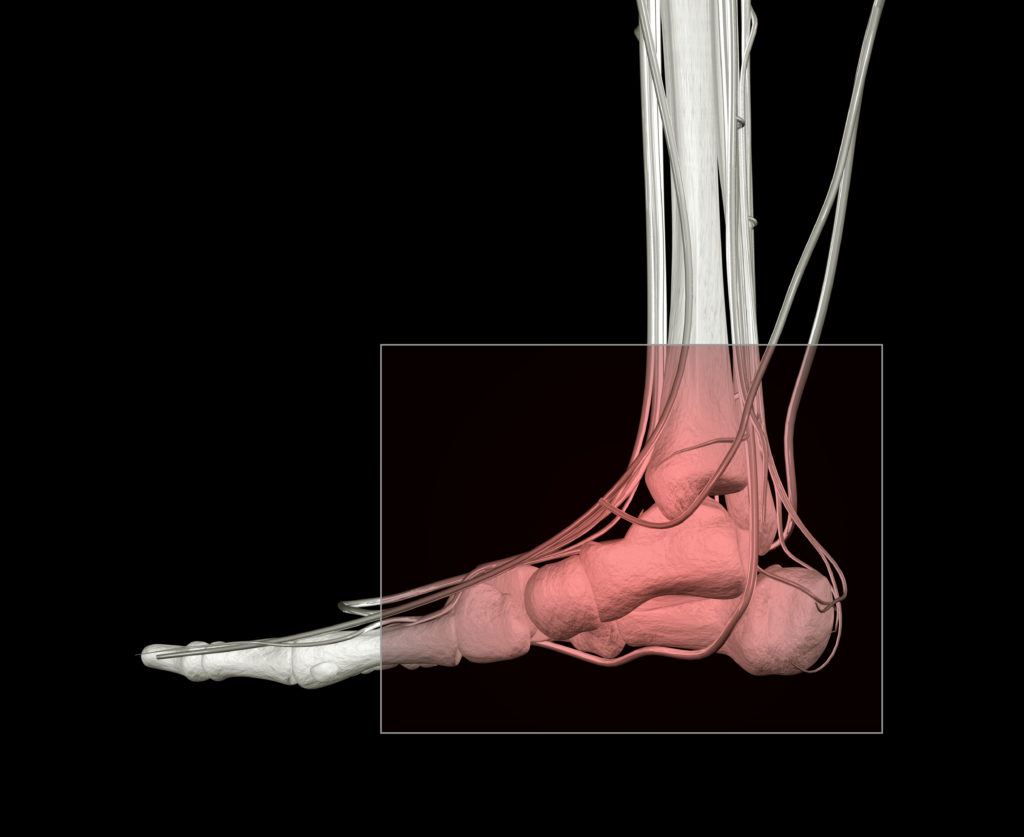
While bursitis can develop at any place in the body where a bursa is located, there are two bursae near the heel that can cause heel pain. The first, known as the retrocalcaneal bursa, is located at the back of your ankle near the heel, where your Achilles tendon meets the end of your calf muscle. The second, known as the Retroachilles bursa, is located between the skin at the back of your heel and the Achilles tendon. When either or both bursae become inflamed and swollen, the condition is known as Retrocalcaneal bursitis or Achilles bursitis.
Common Causes of Retroachilles and Retrocalcaneal Bursitis
Retrocalcaneal bursitis can be caused by many of the same activities that trigger plantar fasciitis or Achilles tendonitis, including overuse from high-impact activities like running or sports that involve a lot of jumping. Uphill running is a particularly high-risk activity for retrocalcaneal bursitis, since the flexed position of the foot during impact means increased contact with the retrocalcaneal bursa. This type of bursitis can also be caused by deformities in the foot, such as Haglund’s deformity, as well as injury or trauma to the foot.
Retroachilles bursitis almost always caused by poorly fitting shoes that rub or dig into the back of your heel. Over time, the Retroachilles bursa becomes irritated, inflamed, swollen, and painful.
Both retrocalcaneal and Retroachilles bursitis are also commonly associated with other conditions that cause trauma to the foot, including Achilles tendonitis, plantar fasciitis, heel spurs, and rheumatoid arthritis.
Symptoms of Retroachilles and Retrocalcaneal Bursitis
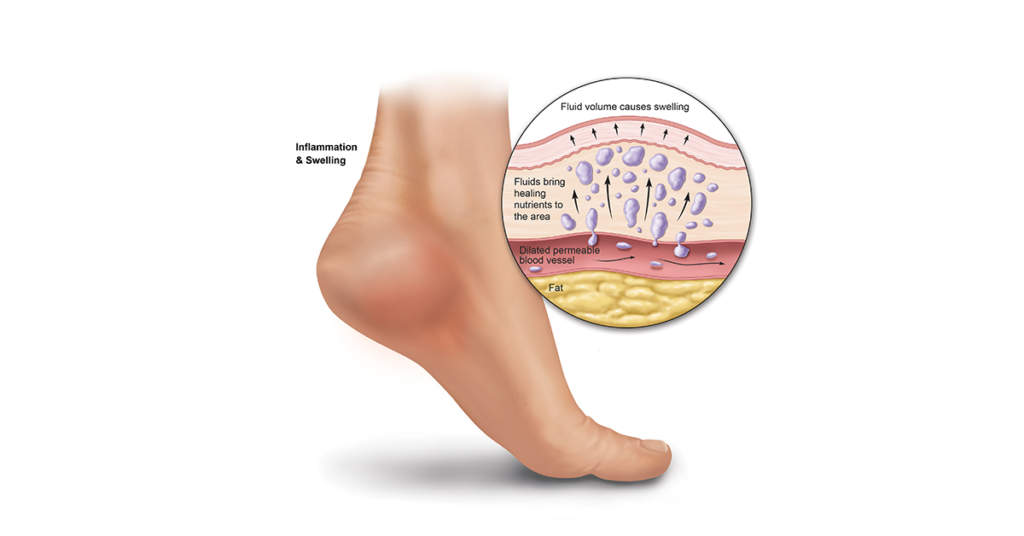
Retrocalcaneal and Retroachilles bursitis can occur at the same time, and the symptoms for both conditions are very similar. Visible swelling is the most common hallmark of bursitis, as well as inflammation, redness, and pain that develops gradually. In the case of Retroachilles bursitis, the swelling may actually present as a hard lump at the back of the heel.
Pain will likely increase if you flex your toes, point your feet downward, or stand on tiptoe since these motions squeeze the bursae.
If you notice any of these symptoms accompanied by a fever, it’s important to seek medical help quickly. While unusual, it is possible for the bursae to become infected and even rupture, a serious condition known as septic retrocalcaneal bursitis.
Bursitis or Heel Pain from Plantar Fasciitis?
While the heel pain associated with retrocalcaneal bursitis or Achilles bursitis can be very similar to the pain from plantar fasciitis, there are a few big differences.
Most importantly, the pain from plantar fasciitis is almost always the worst first thing in the morning, and typically improves somewhat as the fascia stretches and warms up. Heel pain from bursitis, on the other hand, is usually better in the morning, only to get gradually worse throughout the day.
Many stretches that help plantar fasciitis will aggravate an inflamed, swollen bursa. If you think you have plantar fasciitis, but find that stretching makes the pain worse, you may want to consider the possibility that bursitis is involved.
Keep in mind that if you have plantar fasciitis or heel spurs, you may be at greater risk for developing bursitis, because of the overlap in risk factors for bursitis that caused your plantar fasciitis to develop (including ill-fitting footwear and overuse of the feet).
Treatment Options and Advice
The majority of cases of bursitis, especially if addressed properly early on, can be treated successfully in the comfort of your own home. Effective, conservative treatment methods include the following:
- Rest. Take a break from any activity that worsens pain
- Ice. Apply an ice pack several times each day to reduce swelling and inflammation in the bursae
- Use NSAIDs as needed for pain and to decrease inflammation
- Wear supportive, comfortable shoes that keep the heel from rubbing or slipping around. Running shoes, which typically have a protective notch for the Achilles tendon, are especially helpful.
- Orthotic inserts can greatly improve the amount of support and cushioning your feet get as you walk and move, and can also help correct gait abnormalities due to an arch weakness that may be exacerbating the strain on your bursae.
If your heel pain and bursitis do not resolve with these conservative treatments, your doctor may recommend medical treatments such as corticosteroid injections, antibiotics, and surgery as a last resort.
While bursitis can be very painful, the good news is that most cases are successfully resolved without medical intervention. By recognizing the signs and paying attention to your body, you can nip bursitis in the bud before it takes a toll on your feet and health.
7 Heel Spur Myths and Facts
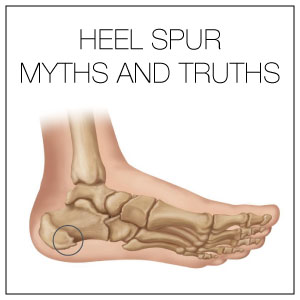 There’s a lot of mystery and misinformation out there about heel spurs.
There’s a lot of mystery and misinformation out there about heel spurs.
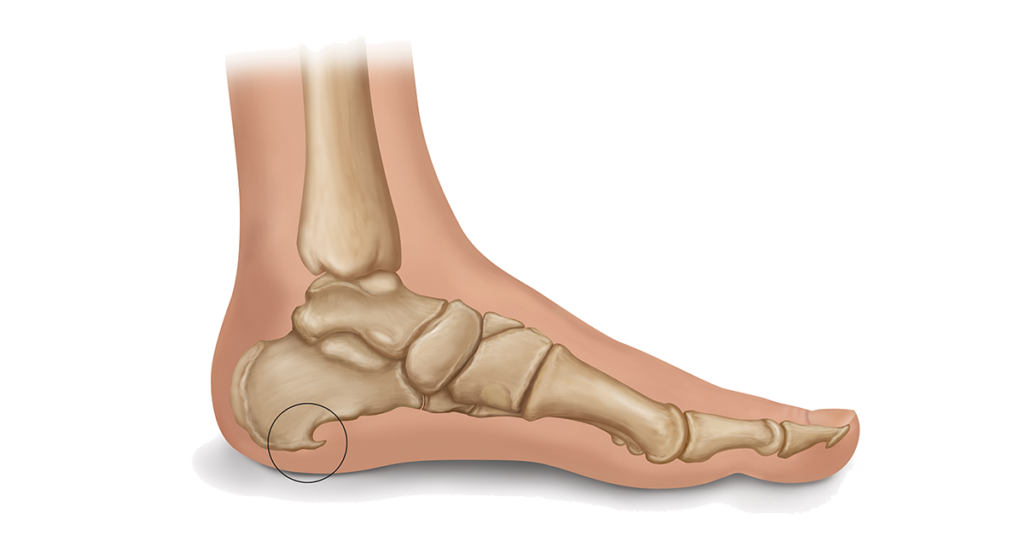
The x-ray photos of tiny white shark-fins protruding into the fatty pad of the heel, combined with the idea of a pointy, painful growth suddenly appearing is more than a little alarming, and foot folklore abounds when it comes to what heel spurs are capable of–and how they can be banished.
So, what’s the true story of these stealthy, sharp intruders?
In this post, we’ll separate fact from fiction and explore some of the most common truths and myths about heel spurs. After all, when you know the real truth about heel spurs, you can take the right steps to treat them!
#1: Can Heel Spurs Break Off?
TRUE. While uncommon, heel spurs do break off now and then, separating from the heel bone and becoming embedded in the foot’s soft tissues. When this happens, you may notice “locking” of the foot when you walk, and additional pain and discomfort.
The best way to avoid breakage is to treat heel spurs as soon as they become apparent through pain, discomfort, and a sharp jabbing sensation in the heel, especially during the first few steps in the morning. Wearing Heel Seats, which raise the arch to a healthy position and take the pressure off heel spurs, can also minimize the chances of breakage.
#2: Can Heel Spurs Be Removed?
TRUE. While surgery is recommended only after conservative treatments have been unsuccessful after at least one year, heel spurs can be removed through surgical intervention.
Guided by a tiny camera, a surgeon can use precise instruments to cut away the bony fragment protruding into the fatty pad of the heel. Heel spur removal surgery is often accompanied by plantar fascia release surgery, which detaches part of the plantar fascia from the heel bone, relieving stress and pressure on the arch.
Even when it’s determined that surgery is the best option to treat heel spurs, it’s important to take preventative steps to keep the heel spurs from returning, by supporting the arch of the foot and providing proper cushioning and impact absorption through high-quality footwear.
#3: Can Heel Spurs Be Dissolved?
UNCLEAR: While you’ll find numerous blog posts and supplements that claim to dissolve heel spurs, there isn’t a lot of scientific research to back these claims. Some suggest that simple apple cider vinegar added to the diet will dissolve heel spurs. Others insist that a deficiency in K2 and D3 vitamins are a contributing cause to the development of bone spurs, and that supplementing with these vitamins will allow the body to naturally dissolve the spurs.
While these natural remedies are generally harmless (as long as you stay within the prescribed daily recommendations for any vitamin supplement), it’s also vital to continue proven treatments for heel spurs, such as icing, rest, stretches, and the use of orthotic shoe inserts.
#4: Can Heel Spurs Move Around?
MOSTLY FALSE. Heel spurs are the result of calcium deposits that cause bony protrusions to grow out of the heel bone. In general, they stay affixed to one spot, although multiple heel spurs may develop on one heel bone.
In rare cases, the heel spur may break off from the heel bone, becoming embedded in the soft tissue and causing additional pain.
#5: Can Heel Spurs Cause Back Pain or Hip Pain?
TRUE. While heel spurs won’t directly cause back or hip pain, they can contribute to and exacerbate it. Heel spurs, especially when left untreated, will cause your gait to change, as you attempt to avoid the pain from the sharp protrusions. Over time, this can lead to misalignment and strain to the hips and back.
#6: Can Heel Spurs Break Through the Skin?
MYTH. While the sharp, piercing pain from a heel spur can, indeed, feel as though the tiny protrusion is trying to break through the skin, heel spurs cannot break through the skin.
When calcaneal heel spurs become very large, it may be possible to feel them beneath the skin; However, there’s no need to fear that the bony protrusion will actually break through the skin.
#7: Can Heel Spurs Make Your Feet Go Numb?
FALSE. As a general rule, heel spurs and plantar fasciitis will cause swelling, redness, and sharp, stabbing pains–but not numbness. If you’re experiencing numbness in one or both feet, Tarsal Tunnel syndrome is a more likely culprit.
Often confused for plantar fasciitis or heel spurs, Tarsal Tunnel syndrome is a result of compression of the tibial nerve and causes numbness and a “pins and needles” sensation, rather than sharp, stabbing pain.
The Truth About Preventing Heel Spurs
Now that you know the truth about heel spurs, you can take effective steps to prevent and treat them. The best way to avoid the development of new heel spurs or damage and pain from existing footwear is to support the arch of your foot properly. After all, a lack of arch support is one of the most common causes heel spurs develop in the first place!
Wear shoes that fit properly and give your heels and arches adequate cushioning and support. Add orthotic inserts to provide an additional boost in support and lift your arch to the optimal height, keeping heel spurs at bay and relieving pain from existing spurs.
It’s also important to maintain a healthy weight and rest your feet often when you’re required to stand for long periods of time.
Think of heel spurs as your foot’s prickly response to an overworked, over-strained arch. By taking care of that arch properly, most cases of heel spurs can be resolved with minimal mystery!