By Dr. Dina Elsalamony MD, MScPH
Despite the stress that we continuously put on our feet through the pressure of various movements and the weight of our bodies, our heels are designed to absorb most of that impact and to provide cushioning to the underlying structures of the feet, including the heel bone (calcaneus), muscles and ligaments. However, heel pain is a very common condition that can negatively impact our ability to bear weight on our feet, causing significant discomfort, interfering with daily activities, and if left untreated for a long period, it can lead to serious complications.
The pain is usually felt under the heel, on the inner or outer side of the heel, or behind the heel. In a lot of cases, heel pain is treated easily with rest, orthotics, or other home remedies, however sometimes the pain and the risk of further damage may persist, requiring more advanced interventions and treatments.
Heel pain can be attributed to numerous reasons, from injury to inflammation to neurological or autoimmune, hence, it is very important to get an accurate diagnosis to ensure an effective treatment that addresses the symptoms in addition to any underlying conditions if present.
In this article, we will provide an overview of the possible causes of heel pain, how it is diagnosed, available treatments, and what measures we can take to prevent it.
Start By Defining Your Heel Pain Symptoms
You may be experiencing a sudden onset of discomfort in one of your feet today, or you may have been trying to ignore recurring foot pain that has bothered you for months or years. The most important first step you can take toward recovery is to spend a few moments thinking carefully about your symptom history. Review the following nine-point list and make a mental note of the symptoms that apply to you.
| True or False: | |
| True or False | The most tender part of my foot seems to be my heel. |
| True or False | My heel hurts most when I get out of bed in the morning. |
| True or False | My heel pain seems worse when I get to my feet after I’ve been sitting down for some time. |
| True or False | The pain in my heel seems to get a bit better after a few minutes of standing or walking. |
| True or False | I walk or run for exercise and one or both of my heels hurt terribly after this activity. |
| True or False | My heel pain seems to be aggravated by the long hours I spend standing at work. |
| True or False | My heel pain is causing me to limp. |
| True or False | I’ve been experiencing this type of pain in my heel on and off for months or years. |
| True or False | I’ve been having periodic bouts of heel pain as I’ve gotten older. |
Understanding your symptoms will help you determine if the cause of your pain is plantar fasciitis or a different condition.
Common causes of heel pain
Some of the common conditions causing heel pain are categorized into the following:
Local conditions that cause heel pain:
Local conditions are conditions that only affect one part of the body, in this case, the heel of the foot.
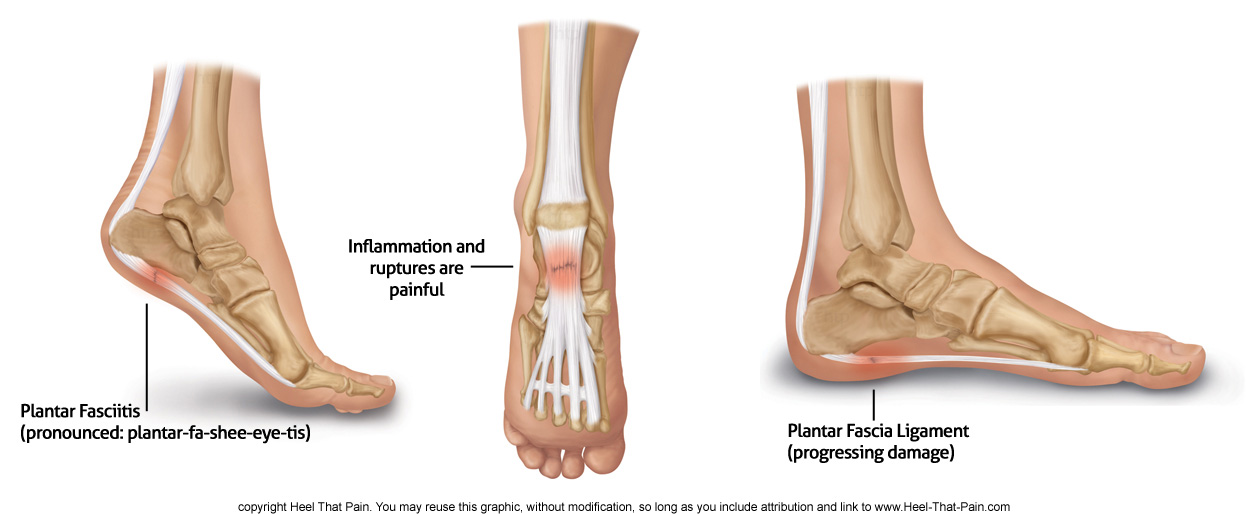
1. Plantar Fasciitis:
This condition is considered to be the most commonly reported cause of heel pain, accounting for 11% to 15% of all foot symptoms requiring professional medical care, it is more commonly diagnosed among athletes, particularly runners with incidence reported as high as 22%. (1) Women also tend to have a higher prevalence than men, for example, in the US, it was found that women are 2.5 times more likely to experience this condition, with the highest incidence occurring between the ages of 45-65. (2)
The plantar fascia is a thick sheath that exists in the bottom of the feet, arising from the calcaneus bone, connecting the heel to the front of the feet. Planter fascia contains type 1 collagen and plays a significant role in ensuring the normal biomechanics of the foot as it acts as a shock absorber and provides cushioning and support to the arch of our feet during walking, running, jumping, or any weight-bearing activity.
Plantar fasciitis is a degenerative disorder, meaning that the fibers of the plantar fascia start degenerating gradually over time. Multiple factors contribute to this outcome, however, overuse and repetitive strain on the feet lead to chronic micro-tearing of the plantar fascia, which is thought to be the most common cause.
Certain populations are at a higher risk of developing plantar fasciitis than others, such as pregnant women, obese individuals, those in occupations that require prolonged standing or weight-bearing actions, runners or athletes, particularly those with a sudden increase in the intensity or duration of their exercise, and those who wear inappropriate footwear.
Individuals with muscular issues, including weak or tight calf muscles, or those with structural problems in the feet such as low/high-arch feet or overpronation, also have a high risk of experiencing plantar fasciitis. The normal process of aging can also pose a risk since it can lead to some degree of fat padding loss leaving the plantar fascia more exposed and susceptible to repetitive microtraumas. Heel spurs are also associated with this condition as they exist in approximately 50% of those diagnosed with plantar fasciitis, however, a heel spur is not the same as plantar fasciitis nor is considered a cause for this condition.
Plantar fasciitis is characterized by pain in the bottom of the feet, involving either the arch or the heel or both, it is usually felt when taking the first few steps in the morning then subsides or disappears after resting or gently walking, however, the pain returns when walking or standing for extended periods of time. The pain is also worsened when walking barefoot or on a hard surface, and for athletes, high-impact fast movements such as sprinting usually increase the intensity of the pain.
Plantar fasciitis is often found in one foot, however, around a third of the cases are diagnosed with plantar fasciitis in both feet.
2. Stress Fracture:
Stress fractures differ from the other regular fractures in the way that stress fracture symptoms, in most cases, are not proceeded by a trauma or a particular incident, as it results from repetitive and recurrent loading of the bone, most commonly in the feet, the calcaneus or metatarsal bones. The normal physiologic response of a bone to increased compression or load is by forming minor microdamage that gets repaired through a process known as remodeling, however, when extensive micro damages occur before the bone had a chance to properly remodel, stress fracture develops. (3) Similar to plantar fasciitis, people may recall changing the intensity, duration, or frequency of their high impact or weight-bearing exercise recently, some of the most common activities that are associated with stress fractures are plyometrics, jumping, running, military training, and gymnastics.
A number of risk factors have been associated with stress fractures, such as low bone density (as in osteoporosis), caloric restriction with lower dietary calcium, females with irregular menstruations, and those who have differences in leg length or muscle weakness. (4) In males, decreased testosterone level has also been considered as a risk factor for stress fractures. (5)
Symptoms of a stress fracture usually have an insidious onset, with the pain associated with a certain activity or when repeatedly loading on the affected foot. The pain can be often accompanied by local swelling or tenderness, and it decreases with rest but returns when resuming the original activity. Sometimes the beginning of the pain can be traced back to a change in training methods or equipment.
Stress fracture makes the bone fragile and if ignored, it can lead to a true fracture. Some stress fractures’ locations, such as the fifth metatarsal, are associated with a higher incidence of certain complications such as non-union (which is the failure of natural healing of broken bones unless surgery is performed).
3. Tarsal tunnel syndrome:
Tarsal tunnel is a condition that involves the tibial nerve or any of its associated branches being compressed or trapped as a result of consistent compression. The tibial nerve runs through a narrow passage inside the ankle called the tarsal tunnel. The compression of the tibial nerve can be a result of one of many causes, including traumas or injuries resulting in changing of the position of the structures around the nerve or swelling which compresses the nerve; high degrees of flat feet can cause also tension on the nerve; diabetic neuropathy; any lesions, masses, tumors or varicose veins around this area which all put more compression on the nerve. (6)
The symptoms of tarsal tunnel syndrome can manifest differently from one person to another; as the pain can be felt either on the bottom of the heel, inside the ankle, or in both area. It can be accompanied by one or more of the following: tingling, numbness, burning sensation, a feeling of electric shock, or pins and needles. These symptoms can either start mildly and gradually then progress, or start abruptly. The pain usually gets worse during physical activity, and in advanced cases, symptoms can also manifest during rest.
Complications can arise if this condition is not treated in time, such as irreversible nerve damage which leads to a permanent impact on the person’s ability to perform everyday activities.
4. Calcaneal bursitis:
Calcaneal bursitis is inflammation of the bursa; which is a structure that resembles a sac and lined by synovial tissue and produces fluid that helps with lubrication and the reduction of friction between various structures like the between tendons or ligaments and bones or between skin and bones. There are 2 bursae located above the entrance of the Achilles tendon, and inflammation to one or both of them will lead to pain in the back of the heel and the ankle.
This inflammation is typically caused by repetitive trauma and overuse, particularly in those who wear inappropriate shoes or tight-fitting ones. Other conditions might also be associated with bursitis such as Haglund deformity, seronegative spondyloarthropathies, rheumatoid arthritis, and gout. (7,8)
The primary complaint presented in this condition is dull aching pain in the back of the heel that is worsened when the person starts a certain activity after rest. Swelling, tenderness, redness, and limping can also occur, and these symptoms can be either unilateral or bilateral.
5. Heel fat pad syndrome:
Fat pad syndrome usually results from the chronic wear and tear of the heel pad fatty tissues, which is responsible for cushioning and supporting our feet bones, leading to changes in the thickness and/or the elasticity of the heel fat pad. Various risk factors play a role in the development of this syndrome, such as aging, repetitive high impact activities, obesity, inappropriate footwear, injury to the heel pad, performing exercises or walking on hard surfaces, having high arch feet, the use of corticosteroid injections as a treatment for other feet conditions, and genetic or family history.
Symptoms associated with heel fat pad syndrome include dull aching pain that usually is felt like a bruise in the center of the heel when walking, running, or standing for long; pain that is recreated by pressing on the center of the heel and is aggravated by coming in contact with a hard surface. In some cases, this condition is mild or asymptomatic, while in some advanced cases the nerves located in the superficial part of the heel are compressed causing some additional neurological symptoms such as pins and needles, tingling, cold, or burning sensation.
6. Haglund’s deformity:
Haglund’s deformity is an abnormality of the foot soft tissues and bone. It is a bony bump appearing on the posterior part of the heel where the Achilles tendon is attached to the heel, and when that large bony bump rubs against shoes, the surrounding soft tissues in the back of the heel become irritated and cause pain.
This condition is also known as “pump bump”, as it was thought at first to affect mostly women who wear high-heeled pump footwear, however, despite having a higher incidence in females than males, it can affect anyone at any age.
The exact cause for that enlarged bony prominent part is not fully known, but a number of potential causes have been linked to this condition, such as heredity, having high arched feet, or having a tight Achilles tendon.
Other risk factors that are thought to aggravate the irritation of bony bump is over-training in athletes and wearing tight, rigid or poorly fitting shoes.
In addition to causing pain, the site of irritation may also get inflamed causing redness, tenderness, and swelling. (9)
7. Heel osteomyelitis:
Osteomyelitis of the heel is an inflammation of the heel due to an infection, resulting from either an injury, surgery, or a bloodstream infection. The infection can be acute or persist for months leading to chronic osteomyelitis. The symptoms of osteomyelitis can be non-specific at times, which leads to delayed diagnosis in some cases. The general symptoms include fatigue, fever, and lethargy, while local and more specific symptoms include heel pain, redness, tenderness, swelling, and decreased range of motion.
8. Achilles tendon issues:
The Achilles tendon is the largest tendon in the human body, consisting of fibrous tissues that connect the heel bone to the calf muscles. A number of problems affect the Achilles tendon causing heel pain, such as:
-
- Achilles tendon rupture: more common among intermittently active people, such as those who exercise mostly during the weekend, and with higher incidence among the ages of 30-50 years old. The symptoms usually are sudden with severe pain resembling the feeling of being kicked or shot in the back of the leg radiating to the back of the heel, another sign of the tendon rupture is the person’s inability to stand on their toes on the affected side.
- Achilles tendonitis: this means an inflammation to the tendon, typically due to overuse, which leads to repetitive microdamage to the tendon without a chance to properly repair, causing degeneration of the tendon or thickening in the paratenon. The pain presents in the back of the heel and the bottom of the calf area, it is usually accompanied by stiffness and tenderness and exacerbated during prolonged activities. Achilles tendonitis is more common among runners, cyclists, gymnasts, tennis players, dancers, and volleyball players.
There are numerous factors that contribute to the injury of the Achilles tendon, for example; repetitive overuse, wearing wrong shoes, changing the intensity of training, having low saddle height in cyclists, family history, rheumatoid arthritis, and some medications such as steroids and fluoroquinolones antibiotics.
9. Sever’s Disease:
Severs disease, more formally known as calcaneal apophysitis, is a condition that is relatively common among active young children, with a higher incidence among boys. (10) Sever’s disease is thought to be due to the fast growth of the heel bone in comparison to the growth rate of the surrounding structures such as tendons, muscles, and ligaments, causing these structures to stretch trying to keep up with the rapid calcaneal bone growth, and if the child is highly active, this adds an additional layer of stress on these structures causing heel pain. The symptoms include heel pain, redness, swelling, tenderness, and trouble walking, the symptoms are worsened with any high impact activity and improve with rest. Symptoms typically manifest around the age of 10-12 for boys and 8-12 for girls.
10. Peripheral Neuropathy:
Peripheral neuropathy is damage to one of the peripheral nerves which are not located in the brain or spinal cord. This condition is either a result of a local cause (trauma to the nerve, tarsal tunnel syndrome, or tumors that are pressing against the nerve), or a systemic cause (diabetes, kidney disease, hypothyroidism, infections). The symptoms associated with neuropathy usually involve burning sharp pain or sensation, tingling, numbness, and in more advanced cases it leads to limb weakness or painless injuries due to loss of the sensation in the feet.
Systemic causes of heel pain:
Systemic causes involve an entire system of the body and may cause heel pain in addition to other symptoms.
1. Rheumatoid arthritis:
Rheumatoid arthritis is a chronic inflammatory condition that is characterized by persistent and symmetric inflammation of the joints, particularly the hands and feet. However, since the inflammation targets the synovial membrane of the joint, it means any joint with synovial lining can be affected. Additionally, as a result of the disease’s systemic and autoimmune nature, other main organs may also become involved such as lungs, skin, heart, and eyes.
The exact cause behind rheumatoid arthritis is not fully understood; genetic, environmental, psychological, immunologic, and infectious factors all play a role in the development and progression of the disease. For example, it is thought that those who are already genetically susceptible, then experience an external trigger such as infection, trauma, or smoking, their immune system sets off series of reactions, leading to inflammation of the joints and impacting other organs.
Symptoms of rheumatoid arthritis usually have an insidious onset, sometimes starting with fever, fatigue, and weakness, before any joint inflammation or pain appears. However, around 10% of people with this condition may show the abrupt onset of joint inflammation and other organ involvement.
The most common symptoms of rheumatoid arthritis include hand and/feet pain particularly around the joints, difficulty performing activities of daily living, pain with motion, tenderness, swelling, deformity of the area affected, and rheumatoid nodules.
Gout:
Gout is another common type of inflammatory arthritis that can cause severe pain, stiffness, and swelling. It is the most common form of inflammatory arthritis among men, although it also affects women, especially after the age of menopause. The cause of this condition is increased uric acid in the bloodstream which then becomes crystalized in the joints, triggering pain and inflammation in the affected joints and the surrounding areas. A number of other conditions are associated with a higher risk of developing gout such as hypertension, obesity, diabetes mellitus, renal insufficiency, anemia, hypercholesterolemia, and hypertriglyceridemia. Certain foods that are high in purines such as anchovies, liver, kidney, sweetbreads, and sardines, increase the risk of high blood serum level of uric acid. It was also found that fructose-rich foods and beverages can increase the risk of gout in both men and women. (11,12) Certain medications and alcohol abuse are other risk factors for developing gout.
Gout attacks tend to start abruptly, particularly at night, and reach maximum severity within 8-12 hours. Symptoms include severe pain, swelling, redness, and tenderness. The most common joint affected by gout is the big toe, it can also affect the ankle, elbows, wrists, fingers, and knee joints. In many cases, heel pain is reported during gout attacks, a study has found that 35% of patients report posterior heel pain, while 20.6% report plantar heel pain. (13)
When to see a doctor for heel pain
It is important to seek urgent medical help if you experience the following, as they are signs of broken bones:
- Severe pain with inability to walk normally.
- Feel dizzy or nauseous from the pain.
- Heard a sound of snap or grinding when the injury happened.
- Your foot or ankle look deformed or at an abnormal angle.
- You have a fever or your foot is very warm as this might be a sign of bone infection.
Alternatively, you can book an appointment with your GP if:
- You have heel pain that hasn’t improved or got worse after 2 weeks of doing at-home treatments.
- You have pain that interferes with everyday activities.
- You experience any tingling, burning sensation, or numbness in the affected foot.
- If you are diabetic.
- Your heel is swollen or stiff.
Heel pain diagnosis:
When you visit a doctor, they will examine your feet, check for any swelling, tenderness, redness, or deformity. They will check your range of motion and leg muscles, and you will be asked about the history of the pain, any medical conditions you have, or family history. Sometimes physical examination is enough to determine the cause of pain, however, if in doubt, or any underlying condition is suspected, a series of other imaging and blood tests will be performed to ensure an accurate diagnosis and appropriate treatment. Each diagnosis comes with a unique code from the ICD-10, which can be used to file insurance claims.
Heel pain treatments:
The treatment of your heel pain will vary based on the diagnosis and whether the cause of the pain is local or systemic, where treating the underlying condition is needed to manage the pain and avoid further complications.
The most common and likely diagnoses are often local and can all be addressed first with conservative treatment, where most people usually recover within a few weeks/months.
Conservative heel pain treatment includes:
1. Rest:
resting is very important in the treatment of many feet orthopedic problems as it allows the tissues the chance to regenerate and recover. This means altering your daily activities to avoid any further tearing or damage. If the pain is severe, full immobilization may be required.
2. Icing:
Icing your heels reduces the inflammation and provides temporary relief of pain, you can apply ice by using an ice bath for your feet, massaging, or ice packs. Heel That Pain provides a more practical and convenient option for icing, introducing the Ice Therapy Slippers which can strap into your feet easily and ice the whole surface area of the bottom of the feet.
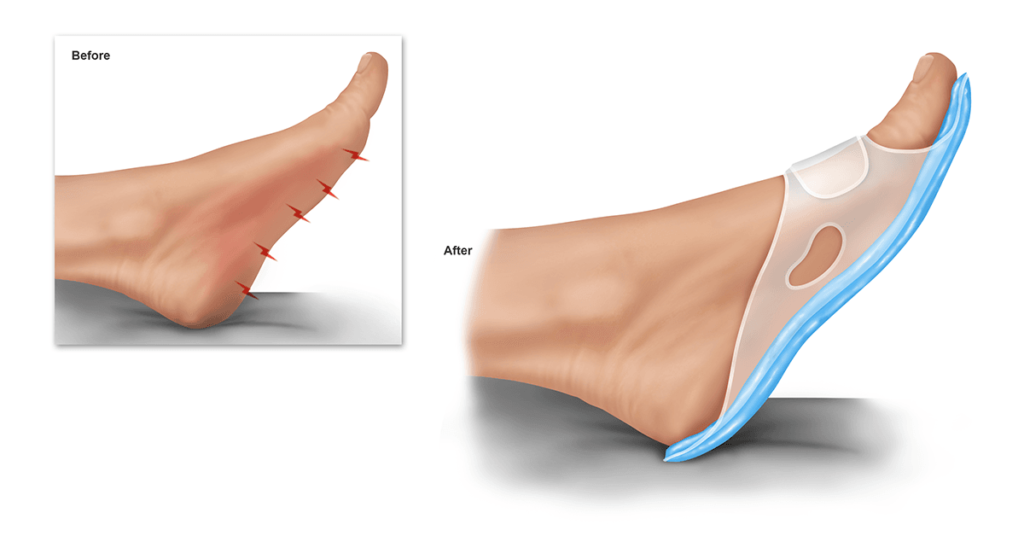
3. Orthotics:
Shoe inserts are considered to be one of the methods used in the first line of management for a number of orthopedic conditions that result in heel pain such as plantar fasciitis, heel fat pad atrophy, Achilles tendon injury, and heel bursitis. Orthotics for heel pain were found to be very effective in reducing the pain even when compared to medications such as non-steroidal anti-inflammatory drugs or cortisone injection. (14) Heel That Pain offers Heel Seat foot orthotics that utilized the revolutionary technology of fascia-bar, providing both shock absorption and strong support to your arch. The dense cushion used in the manufacturing of Heel Seats is made of firm Kraton, which provides the ultimate balance between being gentle on the foot and ensuring strong support, all in an affordable price range.
4. Medications:
OTC non-steroidal anti-inflammatory medications such as ibuprofen or diclofenac can play a great part in reducing pain and managing a number of feet conditions. Antibiotics are used as part of the treatment of osteomyelitis.
5. Night splints:
The night splint is a type of brace that secures your foot in a neutral 90-degree angle position overnight, allowing persistent stretching and elongating of the Achilles tendon and plantar fascia.
6. Shoe change:
Wearing inappropriate shoes that are ill-fitted, rigid, or don’t provide enough support, can contribute greatly to developing foot problems and consequently heel pain. Hence, changing your footwear to high-quality supportive, and perfectly-fitted ones has a great impact on improving your heel pain. In fact, one study found that 14% of its participants mentioned that changing their footwear made the biggest difference in their treatment. (15)
7. Physical therapy and stretching exercises:
Stretching and physical therapy help to improve the tightness of the calf muscles and the Achilles tendon, and strengthen the muscles of the feet.
Medical heel pain treatments
If the person is not responsive to the conservative treatment, more advanced treatments are the next step:
1. Corticosteroid Injections:
If the pain is severe and intolerable or the symptoms do not improve with conservative treatment, injection of corticosteroid may be useful in the management of a number of conditions, such as plantar fasciitis, heel bursitis, and heel bumps. However, caution should be taken with this treatment as it carries some undesirable side effects, particularly in the long term.
2. Surgery:
In most cases, surgery is always saved as a last resort if all other efforts failed to manage the pain or treat the condition. Surgery can be used in the treatment of plantar fasciitis, Achilles tendon injuries, osteomyelitis (in this case as primary treatment in acute cases to drain the pus and save the bone), and heel bumps.
3. Non-invasive procedures:
Various non-invasive procedures are also used to manage some of the cases that are unresponsive to conservative treatment, for example, extracorporeal shock-wave therapy and cryosurgery in the case of plantar fasciitis, or injectable fillers to treat heel fat pad syndrome.
Heel Pain Prevention:
The following tips will help you take care of your feet and avoid heel injury and pain in the future:
- Make sure to wear appropriate shoes for the activity that you are performing.
- Avoid wearing tight, rigid shoes or pointy high heels.
- Make sure to stretch and warm up sufficiently before engaging in any high-impact activity.
- Change your shoes after 250-500 miles, or alternatively try to use supportive orthotics in your old shoes that you can change every few months.
- Avoid exercising on hard surfaces or walking barefoot.
- Make sure to not abruptly increase the intensity or duration of your exercise.
- Allow your body time to heal and recover after high-impact or intense exercise.
- Maintain a healthy body weight to avoid increased pressure and stress on your feet structures.
References:
- Tschopp, M., & Brunner, F. (2017). Erkrankungen und Überlastungsschäden an der unteren Extremität bei Langstreckenläufern [Diseases and overuse injuries of the lower extremities in long distance runners]. Zeitschrift fur Rheumatologie, 76(5), 443–450. https://doi.org/10.1007/s00393-017-0276-6
- https://www.nccih.nih.gov/research/research-results/analysis-of-data-on-the-prevalence-and-pharmacologic-treatment-of-plantar-fasciitis-pain
- Uthgenannt BA, Kramer MH, Hwu JA, Wopenka B, Silva MJ. (2007). Skeletal self-repair: stress fracture healing by rapid formation and densification of woven bone. J Bone Miner, 1548-56. [Medline].
- Popp KL, Hughes JM, Smock AJ, Novotny SA, Stovitz SD, Koehler SM, et al. (2009). Bone geometry, strength, and muscle size in runners with a history of stress fracture. Med Sci Sports Exerc, 2145-50. [Medline].
- Mohamad, N. V., Soelaiman, I. N., & Chin, K. Y. (2016). A concise review of testosterone and bone health. Clinical interventions in aging, 11, 1317–1324. https://doi.org/10.2147/CIA.S115472
- Franson J, Baravarian B. (2006). Tarsal tunnel syndrome: a compression neuropathy involving four distinct tunnels. Clin Podiatr Med Surg, (3):597-609. [Medline].
- Painter C. F. (2008). The classic: inflammation of the post-calcaneal bursa associated with exostosis. 1898. Clinical orthopaedics and related research, 466(7), 1521–1527. https://doi.org/10.1007/s11999-008-0262-z
- Vaishya, R., Agarwal, A. K., Azizi, A. T., & Vijay, V. (2016). Haglund’s Syndrome: A Commonly Seen Mysterious Condition. Cureus, 8(10), e820. https://doi.org/10.7759/cureus.820
- Vaishya, R., Agarwal, A. K., Azizi, A. T., & Vijay, V. (2016). Haglund’s Syndrome: A Commonly Seen Mysterious Condition. Cureus, 8(10), e820. https://doi.org/10.7759/cureus.820
- Wiegerinck JI, Yntema C, Brouwer HJ, Struijs PA. (2014). Incidence of calcaneal apophysitis in the general population. Eur J Pediatr, 173 (5):677-9. [Medline
- Choi HK, Willett W, Curhan G. (2010). Fructose-rich beverages and risk of gout in women. JAMA, 304(20):2270-8. [Medline].
- Choi HK, Curhan G. (2008). Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. BMJ, 336(7639):309-12. [Medline]. [Full Text].
- Roddy, E., Muller, S., Rome, K., Chandratre, P., Hider, S. L., Richardson, J., Blagojevic-Bucknall, M., & Mallen, C. D. (2015). Foot problems in people with gout in primary care: baseline findings from a prospective cohort study. Journal of foot and ankle research, 8, 31. https://doi.org/10.1186/s13047-015-0090-9
- Lynch DM, Goforth WP, Martin JE, Odom RD, Preece CK, Kotter MW. (1998). Conservative treatment of plantar fasciitis. A prospective study. J Am Podiatr Med Assoc, 88:375–80
- Wolgin M, Cook C, Graham C, Mauldin D. (1994). Conservative treatment of plantar heel pain: long-term follow-up. Foot Ankle Int, 15:97–102.