How to Use Compression for Heel Pain
 Massage is a fantastic way to improve symptoms of plantar fasciitis and reduce heel pain. So wouldn’t it be great if you had a tiny personal masseur to ride in your shoe all day?
Massage is a fantastic way to improve symptoms of plantar fasciitis and reduce heel pain. So wouldn’t it be great if you had a tiny personal masseur to ride in your shoe all day?
You’re in luck. Constant, gentle pressure with many of the benefits of massage is exactly the value proposition that compression socks and sleeves provide.
Compression socks and sleeves can be a cost-effective, easy way to improve circulation and reduce pain all day long, and are most effective when used alongside other proven treatment methods like orthotic inserts, icing, and stretching.
Does Compression Really Work?
While there isn’t yet a body of scientific research that confirms the effectiveness of compression in treating the symptoms of plantar fasciitis, there is a significant amount of anecdotal evidence and testimonials.
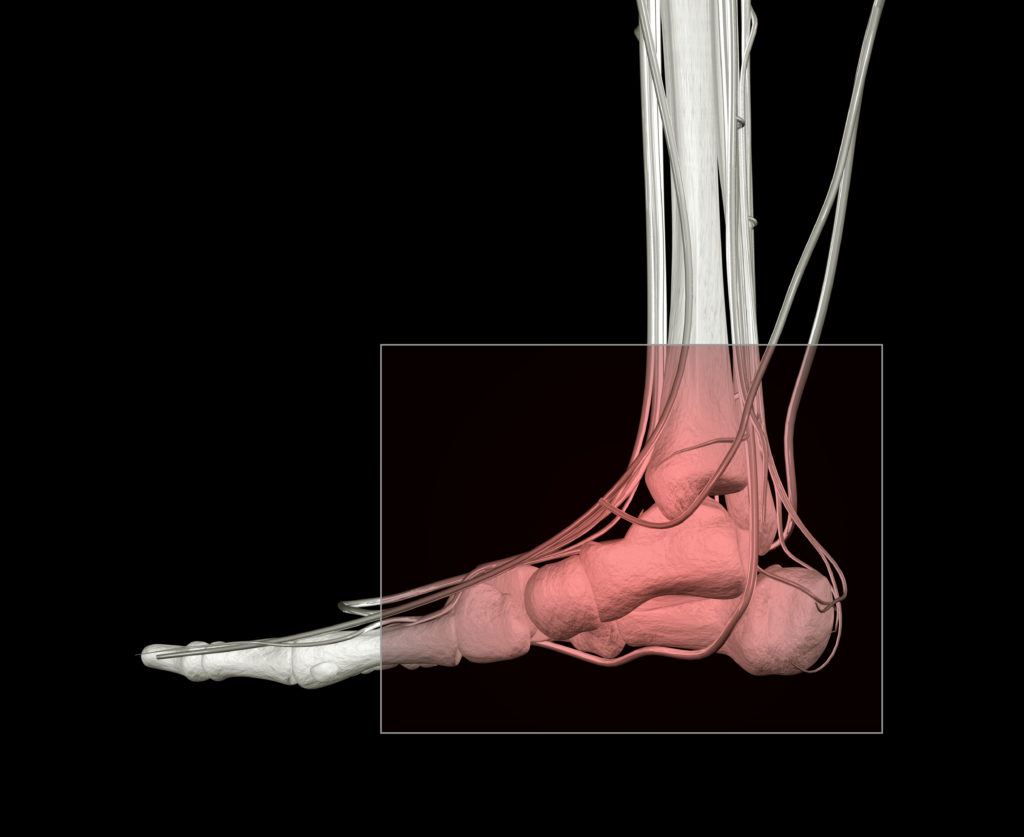
Compression works by applying pressure to specific zones of the heel and foot (most notably the fascia, the ball of the foot, and areas along the ankle) to improve circulation, stretch the fascia, and provide additional support.

Many people find that because compression socks are low-cost, particularly when compared with other treatment options, they’re a viable option to try. If you’ve had positive results from massage and stretching, you may find that compression socks are a good fit for you!
The most common complaints of compression socks and sleeves are an improper fit (either too tight or too loose), tenderness of the heel after use, and not enough support to improve pain. Be sure to find the right size for you, ease into wearing the socks little by little, and combine the socks with additional treatment options.
Look for compression socks and sleeves that are made from moisture-wicking material (to avoid odor or athlete’s foot), and get good reviews from other buyers in terms of comfort, wearability, and durability.
How Compression Helps Plantar Fasciitis
While compression socks and sleeves don’t provide a significant amount of support to the fascia (like orthotics do), they have the unique benefit of working while you’re off your feet. Compression socks can be a great addition to your healing toolbox, particularly if you spend significant amounts of time off your feet.
Even while you are sitting down, the sock or sleeve keeps the foot stable and helps the plantar fascia stay limber and slightly stretched–which can make a big improvement when it comes to those first few steps after inactivity or in the morning! Compression socks and sleeves can also reduce inflammation and swelling through constant pressure.
Compression socks and sleeves can be worn almost anywhere and can stay on while you sleep at night. If the idea of sleeping with socks on drives you crazy, you should know that sleeves are essentially the toeless alternative to compressions socks!
Combining Treatments to Improve Heel Pain

It’s best to think of compression socks as just one part of a treatment regimen. Even if the socks work exactly as designed, your compromised arches will need additional support for true healing to take place.
Compression socks can be used in tandem with orthotic inserts that raise the plantar fascia to the optimal level and provide much-needed support and cushioning that even the thickest socks can’t provide.
Regular icing, stretching, and periodic use of over-the-counter anti-inflammatory drugs are additional staples that you should incorporate if you suffer from heel pain.
If compression socks or sleeves don’t offer quite the support and stretching you’re looking for while you rest your feet, you might also consider sock splints, which can be worn at night and are a softer, more comfortable alternative to night splints.
While compression socks aren’t a cure-all, countless testimonials speak to their effectiveness on an individual basis. They’re low cost, no-risk, and they could be a terrific way to improve your heel pain.
Best Anti Inflammatories for Plantar Fasciitis
By Noelle Ihli, medically reviewed by Dr. Kimberly Langdon, M.D.
 Over-the-counter NSAIDs, or “nonsteroidal anti-inflammatory drugs,” can be an effective way to calm redness, swelling, and pain from plantar fasciitis–particularly if symptoms have been present for less than 6-8 weeks.
Over-the-counter NSAIDs, or “nonsteroidal anti-inflammatory drugs,” can be an effective way to calm redness, swelling, and pain from plantar fasciitis–particularly if symptoms have been present for less than 6-8 weeks.
But are all over-the-counter NSAIDs alike? Which one is best for treating heel pain and plantar fasciitis? And what other treatments should you use in tandem with NSAIDs to heal plantar fasciitis quickly and effectively?
We have your answers!
Are All NSAIDS The Same?
While all NSAIDs reduce swelling, redness, pain, and inflammation, you should be aware of some key differences between popular over-the-counter NSAIDs that you should be aware of. Each type of NSAID will differ in potency, onset time, how long it remains in the body, and how well it blocks prostaglandins (instrumental in causing inflammation).
Ibuprofen (Advil, Motrin)
Ibuprofen is the most common and popularly used over-the-counter NSAID. This drug moderately blocks prostaglandins and has a low risk of GI-tract bleeding and irritation of the stomach lining when used in moderate doses, usually 600 mg every 6 hours.
Naproxen (Aleve)
Naproxen is another popular over-the-counter NSAID that moderately blocks prostaglandins. Like ibuprofen, it has a risk of irritating the stomach lining and causing GI-tract bleeding if used in very high doses, but when used moderately, the risk is very low. Naproxen may cause sensitivity to light.
Ketoprofen (Orudis, Oruvail)
Ketoprofen is another very aggressive prostaglandin blocker and is very effective but should be used with care, since it has a high risk of irritating the stomach and can cause ulcers or gastrointestinal bleeding if used improperly or excessively. Ketoprofen can also cause increased sensitivity to light. These are prescription drugs so your podiatrist or general practitioner will need to recommend these drugs.
Aspirin (Bayer, Ecotrin)
While this NSAID is aggressive in blocking prostaglandins, it carries a low risk of ulcers and irritation of the stomach lining when used in moderation. You should be aware that aspirin can cause respiratory reactions. Do not use aspirin with NSAIDs.
All NSAIDs, if used for long periods of time, can cause kidney damage and eventual damage to the gastrointestinal tract (nausea, bleeding, and vomiting). It’s advisable to use NSAIDS for short periods of time, as needed, to address inflammation and pain.
Which Anti Inflammatory Is Best for Heel Pain?

Anecdotal evidence suggests that ibuprofen is a particularly effective NSAID to address heel pain and plantar fasciitis, because of its high prostaglandin-blocking abilities and low risk of GI-irritation when used in moderate doses.
It’s important to understand that every person responds differently to different NSAIDs, and it’s a good idea to experiment with different over-the-counter NSAIDs to find the one you like best. Depending on the severity of your pain and your experience with over-the-counter NSAIDs, your doctor may also recommend trying more powerful prescription NSAIDs.
Acetaminophen or Tylenol can help ease the pain but has minimal anti-inflammatory effects.
Anti Inflammatories as a One-Two Punch

While NSAIDs are both effective and useful, it’s critical to understand that they aren’t a miracle cure–or a cure at all. NSAIDs effectively–but temporarily–reduce pain, swelling, and inflammation. The underlying cause of plantar fasciitis and heel pain must be addressed for true healing to take place.
The good news is, 90% of plantar fasciitis cases can be resolved with conservative, at-home treatment methods, particularly if symptoms are addressed early! Since all NSAIDs carry the risk of GI-irritation and other negative side effects if used to excess, it’s important to investigate and use sustainable treatments for plantar fasciitis and heel pain that not only relieve pain but strengthen and heal the plantar fascia itself.
Commit to treatment methods like stretching, icing, rest, and wearing special orthotic inserts that treat your pain while keeping you active.
There’s little question that NSAIDs are a terrific tool for temporarily addressing heel pain and paving the way for other conservative treatment methods. Remember to moderate your use of these helpful drugs, and to use them in tandem with treatments that address the underlying cause of your heel pain.
Dry Cupping for Plantar Fasciitis
 If you watched the Rio Olympics, you probably remember the sensation caused by the deep red circles seen on the backs and shoulders of many athletes.
If you watched the Rio Olympics, you probably remember the sensation caused by the deep red circles seen on the backs and shoulders of many athletes.
These circles, evidence of dry cupping, led to a renewed interest in the alternative therapy; however, it’s important to understand that dry cupping has been used by many cultures, for many thousands of years to treat pain, increase blood flow, loosen stiff muscles, and even improve degenerative disorders.
Because of its low cost and effectiveness at reducing pain, dry cupping has surged in popularity as a conservative alternative to medical intervention, especially in severe or very persistent cases of plantar fasciitis.
Thinking about giving dry cupping a try? Here’s what you need to know!
What Is Dry Cupping?
Dry cupping is a manual therapy that involves positioning a cup on the skin and creating a vacuum to apply negative pressure. This negative pressure increases blood flow to the area. Dry cupping can be done with either a heated cup that creates a vacuum as it cools, or a simple system involving a cup and a manual hand pump, which creates the negative pressure once the cup is applied. Dry cupping can either be done with a physical therapist or at home, using kits that may be purchased for a small amount (approximately $35).

Cups remain on the skin for between five and ten minutes, after which they are carefully removed. As the skin is raised through suction, increased blood flows through the cupped area, which can reduce pain as well as break up adhesions if they are present.
Dry cupping has been used to treat conditions like fibromyalgia, carpal tunnel syndrome, osteoarthritis, and chronic pain in the neck, back, and shoulders. Recently, dry cupping has also been studied as a potential treatment for plantar fasciitis.
Dry Cupping for Plantar Fasciitis
While numerous studies have been conducted on the effectiveness of dry cupping as a pain management therapy, most studies about dry cupping and plantar fasciitis specifically are still forthcoming. However, one recent study revealed a correlation between dry cupping and pain reduction for plantar fasciitis, particularly when combined with electrical stimulation therapy.
This study found that dry cupping, when combined with electrical stimulation therapy (such as TENS therapy), was very effective in significantly reducing plantar fasciitis pain for the majority of participants. Participants reported reduced overall pain, and reduced morning pain as a result of two sessions of dry cupping per week, for four weeks.
It can be helpful to think of dry cupping as the opposite of myofascial massage. Instead of applying positive pressure to the fascia by massaging the damaged tissue, dry cupping applies negative pressure to the plantar surface, heels, and calves, allowing more blood to circulate and help promote healing and loosen the muscles and ligaments in these areas.
Side Effects and Considerations for Dry Cupping

This file is licensed under the Creative Commons Attribution 4.0 International license via WellcomeImages.
Side effects of dry cupping are minimal and include temporary, raised red circles on the skin, slight swelling, and sometimes a mild pinching sensation as the vacuum applies negative pressure.
It’s important to apply the cups only to soft tissue, not bone. It’s also important not to leave the cups on the skin for extended periods to avoid skin damage or broken capillaries. Cupping isn’t recommended as a treatment for pregnant women, individuals with deep vein thrombosis, conditions that cause broken or irritated skin, or individuals with certain types of spreading cancers.
It’s also important to remember that cupping is best used in tandem with proven conservative treatments for plantar fasciitis, such as icing, stretching, weight loss, and orthotics made for plantar fasciitis. Experimenting with low-risk, conservative treatment methods while sticking with these basics can be a great way to find new and helpful pain-management techniques, and ultimately, healing.
TENS Therapy for Plantar Fasciitis
 TENS therapy, which stands for “Transcutaneous Electrical Nerve Stimulation,” uses a low-frequency electrical current to stimulate the plantar fascia, with the goal of improving blood flow and blocking the body’s pain signals.
TENS therapy, which stands for “Transcutaneous Electrical Nerve Stimulation,” uses a low-frequency electrical current to stimulate the plantar fascia, with the goal of improving blood flow and blocking the body’s pain signals.
While this therapy is more costly than other more conservative, noninvasive methods for treating plantar fasciitis at home (simplified options are closer to $50, while higher-end products fall in the neighborhood of $250), some of the cost may be covered by your insurance! TENS therapy is also far less expensive and risky than surgery or other medical interventions.
Here’s what you should know about TENS therapy before you give it a try for foot pain!
TENS Therapy and Foot Pain
TENS therapy works by attaching electrodes to the feet (and sometimes calves) that deliver very small pulses of electrical current. This current causes the muscles in the feet and legs to contract and release at intervals, which is designed to improve blood flow as well as interrupt the body’s signals for pain. You’ll feel a gentle pulsing sensation, as well as some vibration in the soles of your feet while the device is working. Some TENS devices look like a pair of sandals that you slip onto your feet, others look like a cell phone with electrodes attached, while still others look like a small platform that you place your feet.

There’s a lot of anecdotal evidence that TENS therapy helps reduce inflammation, reduces stiffness and pain to the plantar fascia, and reduces pain while walking and other physical activity. However, it’s important to understand that TENS therapy is not intended to be a cure for plantar fasciitis–but rather a pain-reduction method.
Does TENS Therapy Work?
The number one question on everyone’s mind is, of course, does TENS therapy work? While the answer isn’t as conclusive as you might like, there’s still good news: One major study, which separated plantar fasciitis sufferers into two groups (one that only used stretching and orthotics, and one that used stretching, orthotics, and low-frequency electrical stimulation therapy) found that both groups reported significantly less morning pain and overall symptoms of plantar fasciitis. In other words, if you want to give TENS therapy a try, you can feel confident that, as long as you combine this therapy with tried and true treatments like orthoses and stretching, you’ll be setting yourself up for success.
Many companies offer a money-back guarantee, so you can try before you fully commit to the investment of TENS therapy. Make sure to read the warranty and guarantee information carefully before purchasing.
TENS vs ESWT
While TENS therapy and ESWT therapy (extracorporeal shock wave therapy) might seem similar, since they both use electrical currents, the two procedures are different in several ways. ESWT is far more expensive (nearly $1000 before insurance in many cases), and must be done by a licensed professional in a doctor’s office. It’s also more painful, and can cause intense discomfort, redness, and swelling.
Like TENS therapy, ESWT hasn’t been proven, and studies of its effectiveness are limited and mixed. For many people TENS therapy is a cost-effective, at-home way of experimenting with the results of electrical current on their plantar fasciitis.
Is TENS Therapy Safe?
TENS therapy can be done at home with a portable unit, has minimal risks, and is considered very safe. As with all forms of muscle work, make sure to keep yourself hydrated while using TENS therapy, to avoid fatigue and any buildup of toxins that may be released during muscle stimulation.
It’s also important to pace yourself while using TENS therapy. Some people have reported muscle tightness and discomfort after prolonged periods of use, or if the setting is too high. Work up to longer sessions gradually, and avoid using TENS therapy for long periods of time.
Since TENS therapy uses electrical current, you shouldn’t use it if you have a pacemaker. If you’re pregnant or have other medical complications, make sure to consult your doctor before starting TENS therapy.
Whether you choose to give TENS therapy a try, or not, remember that 90% of plantar fasciitis cases can be resolved with a little time and consistent, conservative treatment. Along with any pain-reduction methods you try, make sure to use tried and true orthotics for plantar fasciitis, stretching, and icing to address the root cause of your foot pain. Here’s to the health of your feet!
What To Do When Plantar Fasciitis Won’t Go Away
 While the fact that 90% of plantar fasciitis cases can be resolved with conservative at-home treatment, if you’re one of the 10% whose plantar fasciitis doesn’t respond to natural remedies–and perhaps even gets worse–it can be discouraging, to say the least.
While the fact that 90% of plantar fasciitis cases can be resolved with conservative at-home treatment, if you’re one of the 10% whose plantar fasciitis doesn’t respond to natural remedies–and perhaps even gets worse–it can be discouraging, to say the least.
Everyone is different. And if you’ve exhausted the options for conservative treatments like rest, icing, stretching, and support from orthotic inserts over nine months to one year, it’s time to consider more advanced treatment options with your doctor.
What are your options when plantar fasciitis won’t go away, and what can you expect in terms of options, costs, and special considerations?
The good news is, there are several effective options to explore with your doctor.
Advanced Treatment Options for Plantar Fasciitis
There are many treatment options for advanced plantar fasciitis that gets worse or doesn’t respond to conservative treatments. However, take heed of separating anecdotal evidence (you’ll find an abundance!) in favor of research. The following are the most popular advanced treatments for stubborn cases of plantar fasciitis:
Ultrasound Therapy:
Ultrasound therapy essentially works by vibrating and stimulating tissues and cells. It’s relatively painless, simple, and less expensive than many other advanced therapies. However, while some people sing the praises of this advanced treatment for stubborn plantar fasciitis, the evidence of its effectiveness is meager at best.
Extracorporeal Shockwave Therapy (ESWT):
ESWT is more expensive (often close to 200 dollars per visit) and significantly more painful than standard ultrasound therapy. Several studies have concluded it seems to be effective for treating stubborn cases of plantar fasciitis; however, there by no means is a consensus among doctors or patients.
Platelet-Rich Plasma Injections:

In this therapy, your own platelet cells are centrifuged and then injected into the damaged plantar fascia. And while this therapy has become very popular among certain athletes for a variety of injuries, its effectiveness hasn’t been proven. It’s also expensive–running upwards of $300 per injection.
Corticosteroid Injections:
Cortisone, a powerful anti-inflammatory, is generated naturally by your body in response to stress. Corticosteroid injections use a synthetic version of cortisone and are injected directly into the heel. While these injections appear to have high rates of success for short-term relief (several weeks), long-term effects are unclear. The cost of one injection can range from $100 to $300; a series of three shots is the typical prescription.
Radiation Therapy:
Radiation therapy, often used in the treatment of cancer, has been shown to be an effective treatment for some stubborn cases of plantar fasciitis. This therapy is also on the lower end of cost, has minimal side effects and risks, is simple and non-invasive, and is not painful. The procedure similar to getting an x-ray. One 2012 study found that 80 percent of patients experienced complete pain relief following the therapy, and 64 percent were still pain-free 48 weeks later.
Intracorporeal pneumatic shock therapy (IPST):
This new therapy is similar to ESWT and applies shock waves to heel spurs. It requires local anesthesia and is less painful than ESWT. One study showed a 92% success rate in pain reduction reported by patients. It’s also less expensive than ESWT.
Numerous Surgical Options:
While surgery should be considered as a last resort for advanced disease because of its cost and potential complications, it may be a good choice if other treatment methods fail. Many types of surgery for plantar fasciitis have high success rates but require significant time off your feet, high costs, and pain.
Finding a Plantar Fasciitis Doctor
It can be a challenge to find a family doctor who is prepared to treat severe or chronic cases of plantar fasciitis. Many people who suffer from plantar fasciitis that does not respond to treatment seek the help of a podiatrist, who specializes in feet. However, not all podiatrists are alike. Some may lean more heavily on surgical options, while others take a more graduated approach. Search medical forums like ratemds.com and patient forums dedicated specifically to plantar fasciitis for recommendations and insight before you make a commitment to a particular doctor. If you find that you’re not aligning with a particular doctor, don’t be afraid to make a change. It might be a hassle, but your peace of mind and healing are worth it!
Managing Chronic Heel Pain

Many advanced treatment options for plantar fasciitis are administered over a period of time. During treatment, it’s important to have go-to options for pain management that help you find relief and stay positive. Working with your doctor, you may find that the following pain-management tools are helpful while you undergo advanced treatment for plantar fasciitis:
- RICE: Conservative methods used to treat plantar fasciitis can still be used as tools to manage pain, even while exploring more advanced treatment options. RICE, or rest, icing, compression, and elevation will help improve circulation, numb pain, and reduce inflammation.
- Orthotic Inserts: Orthotics made especially for plantar fasciitis not only provide cushioning but lift the heel and arch so that heel spurs (a major source of pain in many cases of plantar fasciitis) don’t dig into the heel. Click here to get doctor-recommended orthotic inserts.
- Night Splints: Using a night splint, which gently and comfortably stretches the heel and arch while you sleep, can help take the bite out of morning pain.
- Self-Massage: Applying gentle pressure while rolling a mobility ball or golf ball beneath your heel and arch can stimulate blood flow and reduce pain.
- Stretching: A variety of stretches for the heel and foot can improve flexibility and strength in the arch, as well as reducing morning pain.
- Over-the-Counter Anti-Inflammatory Drugs: Anti-inflammatories like ibuprofen can reduce inflammation and pain as needed. Just be sure to follow dosing instructions and consult with your doctor when taking these drugs long-term, since overuse can harm the lining of your stomach.
While conservative treatments for plantar fasciitis are appealing because of their effectiveness and low cost, there are cases in which advanced treatments and even surgery may be the right choice for you. By understanding your options, working with a trusted doctor to create a plan, and using pain-management techniques, you can look forward to a brighter future that doesn’t revolve around foot and heel pain.