What is Plantar Flexion?
 What does Swan Lake have in common with a jog down the beach?
No, we’re not talking about birds (but keep an eye on that flock of seagulls). We’re talking about plantar flexion.
The same movement that allows ballet dancers to stand en pointe allows your foot to bend at the ankle when you take off during a run, especially through a shifting surface like sand. Plantar flexion is the opposite of dorsiflexion (when your foot bends upward) and takes place any time your foot bends downward. for example, when you stand on tiptoe or press down on the pedal of a sewing machine or the brakes in your car.
As with any movement your body makes, it’s possible to sustain injury through plantar flexion. How does plantar flexion relate to plantar fasciitis and other foot injuries, and how can you prevent and address these potential risks?
Read on!
What does Swan Lake have in common with a jog down the beach?
No, we’re not talking about birds (but keep an eye on that flock of seagulls). We’re talking about plantar flexion.
The same movement that allows ballet dancers to stand en pointe allows your foot to bend at the ankle when you take off during a run, especially through a shifting surface like sand. Plantar flexion is the opposite of dorsiflexion (when your foot bends upward) and takes place any time your foot bends downward. for example, when you stand on tiptoe or press down on the pedal of a sewing machine or the brakes in your car.
As with any movement your body makes, it’s possible to sustain injury through plantar flexion. How does plantar flexion relate to plantar fasciitis and other foot injuries, and how can you prevent and address these potential risks?
Read on!
Injuries and Pain Related to Plantar Flexion
 Plantar flexion engages the joints at your ankle, the muscles in your calf and ankle, and the arch of your foot. All of these areas absorb impact as the foot pushes downward to propel you forward while running, or lift the weight of your body when you stand on tiptoe. That impact and stress can wear on the muscles and ligaments involved in plantar flexion.
Plantar fasciitis is one of the most common injuries associated with plantar flexion, particularly in runners or other high-impact sports that involve plantar flexion, such as ballet. Overuse and strain to the arch as the foot flexes can create inflammation and small tears in the plantar fascia that lead to pain.
Other injuries that can result from plantar flexion include sprained ankles and pulled muscles in the calf and legs, Achilles tendonitis, and shin splints. Running or jogging on uneven or shifting surfaces like sand can increase the risk of strain and injury to the fascia and the muscles of the calf and feet.
Plantar flexion engages the joints at your ankle, the muscles in your calf and ankle, and the arch of your foot. All of these areas absorb impact as the foot pushes downward to propel you forward while running, or lift the weight of your body when you stand on tiptoe. That impact and stress can wear on the muscles and ligaments involved in plantar flexion.
Plantar fasciitis is one of the most common injuries associated with plantar flexion, particularly in runners or other high-impact sports that involve plantar flexion, such as ballet. Overuse and strain to the arch as the foot flexes can create inflammation and small tears in the plantar fascia that lead to pain.
Other injuries that can result from plantar flexion include sprained ankles and pulled muscles in the calf and legs, Achilles tendonitis, and shin splints. Running or jogging on uneven or shifting surfaces like sand can increase the risk of strain and injury to the fascia and the muscles of the calf and feet.
Stretching to Improve Plantar Flexion
It’s possible to improve the flexibility and strength of the critical muscles and ligaments involved in plantar flexion through simple stretches in the comfort of your own home. Stretches that work the heel, calf, and arch greatly reduce your chances of injury or pain during plantar flexion. This includes stretches like toe walking, calf raises, and box jumps, which increase the strength and flexibility of the calves and feet, allowing them to absorb impact more effectively and withstand more stress. Make it a habit of incorporating these stretches in your daily routine, particularly if you’re a runner or participate in high-impact sports. Find the stretches you enjoy the most, and use them regularly throughout the week and prior to workouts.
If you do experience pain during plantar flexion, give yourself a break from the activity that is causing the pain. Icing and taking anti-inflammatories like ibuprofen, while building up greater strength and flexibility in the muscles and ligaments of the feet and legs through stretching, can also be used to address the pain at home. However, if you continue to experience pain during plantar flexion, be sure to consult your doctor.
Make it a habit of incorporating these stretches in your daily routine, particularly if you’re a runner or participate in high-impact sports. Find the stretches you enjoy the most, and use them regularly throughout the week and prior to workouts.
If you do experience pain during plantar flexion, give yourself a break from the activity that is causing the pain. Icing and taking anti-inflammatories like ibuprofen, while building up greater strength and flexibility in the muscles and ligaments of the feet and legs through stretching, can also be used to address the pain at home. However, if you continue to experience pain during plantar flexion, be sure to consult your doctor.
The Right Shoes for Proper Plantar Flexion
Another important part of healthy plantar flexion and avoiding injuries like plantar fasciitis or muscles strain is wearing the right shoes. You may have noticed that many running shoes have a flexible, softer toe box. Wearing shoes that allow the foot to flex naturally, while supporting your arch and heel with a thick, cushioned sole will go a long way to help you avoid injury and pain. To add additional support and cushioning to your favorite running shoes, consider adding orthotic inserts. Giving your arch extra support will help absorb the impact of running or physical activity more effectively, reducing strain to the muscles and ligaments required for dorsiflexion. Most of the time, there’s no need to think about plantar flexion. It’s just one of the many movements our bodies coordinate, allowing us to move and play in an astonishing variety of ways. But staying aware of potential injuries to this everyday motion can mean the difference between effortless motion and injury!10 Little-Known Heel Spur Facts
Heel spurs: Think of them as the great whites of the feet. Stealthy, with a sharp little fin that can surface and cause a lot of pain and damage.
What do we really know about this painful condition that can lurk below the surface of your feet?
We’ve compiled some of the most interesting facts and statistics about heel spurs to help you learn what they’re really all about. Because, like great whites, they’re a lot easier to handle, coexist with, and avoid when you understand a little more about them!
Reduce heel spur pain with our 100% guaranteed Heel Seat inserts!
1. Heel Spurs Can Cause Morning Heel Pain
If you have plantar fasciitis, you’re all too familiar with morning pain–those first excruciating steps after getting out of bed. Why? Heel spurs are often enemy #1 as they dig into already-tender tissue for the first time after a period of inactivity.
2. Heel Spurs Become More Common As We Age
Studies across the board reveal that heel spurs are far more common in both men and women as they age. Large heel spurs are much more prevalent in people who are older than 40.
3. Heel Spurs Don’t Always Cause Pain

Approximately 38 percent of the population has a heel spur–but many don’t even know it! One study that spanned 45 years found that that heel spurs weren’t ever the cause of pain for many people who had them.
4. Heel Spurs are Common in Plantar Fasciitis Sufferers
While heel spurs and plantar fasciitis don’t always go hand in hand, About 70 percent of people with plantar fasciitis do have painful heel spurs. It’s thought that the body creates heel spurs as a protective measure in response to damage to the plantar fascia.
5. Heel Spurs are the Body’s Attempt to Protect the Fascia
Interestingly enough, researchers believe that heel spurs are actually the body’s attempt to protect the plantar fascia and other tissue from damage and strain. When damage occurs, cells are called to the area and begin depositing calcium. Over time, these deposits can build up into sharp protrusions that hurt, not help.
6. Heel Spurs Can Occur In Different Places
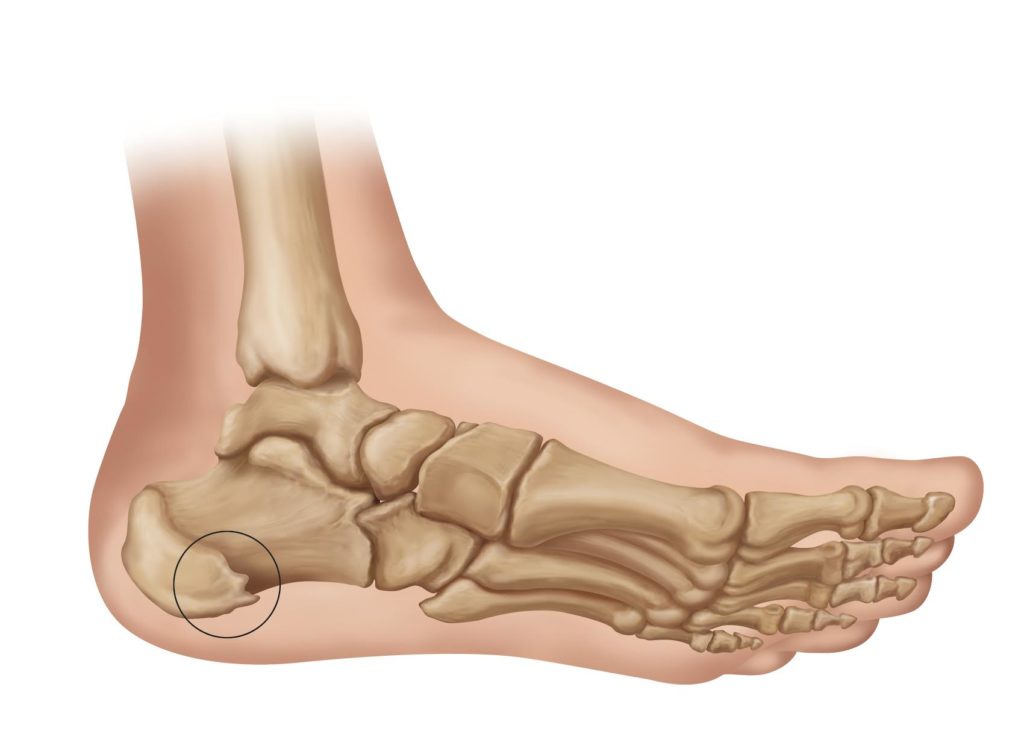
Heel spurs form on the bottom of the heel, while bone spurs caused by Achilles tendonitis form along the back of the heel. Despite the fact that these conditions are different, studies have found a moderate correlation between them.
7. Women Are More Likely to Develop Heel Spurs
Ladies aren’t so lucky when it comes to heel spurs. Studies find that women are more likely to develop heel spurs than men. Why? Some have theorized that it’s because of the types of shoes women are more likely to wear, which can damage the plantar fascia and cause heel spurs.
8. The Connection Between Heel Spurs and Osteoarthritis
Heel spurs are also more common in individuals with Osteoarthritis, the most common form of arthritis. This degenerative condition erodes away the cartilage at the joints. As the body scrambles to compensate for the loss of cartilage, it may develop painful bone spurs
.
9. Weight and Heel Spurs
There’s also a connection between individuals who are overweight and the development of heel spurs. Since more weight means more impact and strain to the arches of the feet and the tissue of the heel, damage is more likely as well–which can trigger the onset of heel spurs.
10. Hope for Recovery
The good news is that 90 percent of people who experience painful heel spurs are able to recover without surgical intervention, by changing their footwear, addressing causes like plantar fasciitis using orthotic inserts, and even taking supplements that help the body more effectively use nutrients and minerals.
While heel spurs can still be an unsettling and painful condition, the more you know about their causes, symptoms, and treatment, the more equipped you’ll be to manage them!
What is Plantar Fibromatosis?
 Plantar fibromatosis, also known as Ledderhose’s disease, is a condition that causes benign, slow-growing nodules to form along the fascia of the foot.
Plantar fibromatosis, also known as Ledderhose’s disease, is a condition that causes benign, slow-growing nodules to form along the fascia of the foot.
The nodules may grow slowly, undetected for months or even years at a time, followed by sudden, rapid growth. As time passes and the nodules grow, walking may become uncomfortable or painful.
While this condition sounds scary, it is relatively rare, and the nodules are almost never malignant. How will you know if the symptoms you’re experiencing are plantar fibromatosis? What causes this condition? Is plantar fibromatosis related to plantar fasciitis? And what are your options for treatment if you are diagnosed with plantar fibromatosis?
Here’s what you need to know:
Plantar Fasciitis vs. Plantar Fibromatosis
While both plantar fasciitis and plantar fibromatosis revolve around the fascia of your feet, the causes of the two conditions are typically considered to be very different. Plantar fasciitis is caused by overuse and trauma to the arch of the foot, while researchers believe that the primary cause of plantar fibromatosis is rooted in genetics.
While there are some researchers who believe that plantar fibromatosis can be triggered by the body’s healing response to a tear in the fascia–a possible connection to plantar fasciitis–this link has not been proven. It is, however, just one more good reason to take good care of your arches!

Regardless, it is possible to have both plantar fasciitis and plantar fibromatosis at the same time. And, depending on the location and severity of the nodules caused by plantar fibromatosis, orthotic inserts that lift, cushion, and support the arch of the foot may be an effective, non-surgical way to make walking and physical activity more comfortable.
Causes of Plantar Fibromatosis
Researchers are still working to understand the exact cause of plantar fibromatosis, but the general consensus is that the condition is genetically inherited. In other words, if someone in your family has this condition, you’ll want to pay special attention to the symptoms listed below. As with many genetic disorders, the genes for plantar fibromatosis can be influenced by a number of factors which increase the likelihood that you’ll develop this condition.
Risk factors for plantar fibromatosis may include alcoholism, smoking, and chronic stress to the feet. There also appears to be a connection between plantar fibromatosis and epilepsy, thyroid conditions, palmar fibromatosis (a condition affects the connective tissue in the hands), and diabetes. Men develop plantar fibromatosis more often than women.
Symptoms of Plantar Fibromatosis
Because the nodules from plantar fibromatosis develop so slowly–and may event stop growing altogether and become dormant for months and years–many people aren’t aware that they have this condition for many years.
Usually, the first symptom is a small, painless lump on the sole of the foot. In most cases, this lump appears that the highest part of the arch. Walking or physical activity may become uncomfortable of painful as the lump grows and rubs against your shoes or the ground as you walk.
Usually, you’ll only notice this lump in one foot. Only a small percentage of people who have plantar fibromatosis experience the condition in both feet at once.
Diagnosis and Treatment of Plantar Fibromatosis

If you notice symptoms that might indicate plantar fibromatosis, your doctor will likely recommend an MRI or sonogram as a first step. This will help you and your doctor see the extent of the plantar fibromatosis and determine next steps in treatment.
If the nodule(s) are small, your doctor will recommend that you avoid direct pressure, and may also recommend orthotic insoles that cushion and support your arch and relieve pressure to the nodules.
If conservative treatments aren’t effective, or if the nodules continue to cause pain while walking, your doctor may recommend radiotherapy to reduce the nodules’ size. The side effects of radiotherapy are minor, and this treatment has been shown to be approximately 80% effective (Panizzon & Seegenschmiedt, 2014).
Other non-surgical treatment options that you and your doctor may explore include cortisone injections and collagenase injections.
Surgery is usually recommended as a last resort, and only if the nodules cause unmanageable pain. Because the nodules are typically so closely situated to muscles, nerves, and tendons, it can be very difficult to remove all of the nodules. And any portion of the nodules that remain in the foot will continue to grow. Surgery also has a long recovery time and can be very costly.
There’s nothing more unsettling that discovering a lump on the foot. And while the symptoms of plantar fibromatosis can be disconcerting, the good news is that most cases can be managed effectively at home, without surgery. Recognizing the symptoms, understanding your options for treatment, and then working with your doctor to determine how to best manage this condition will help get you back on your feet and in control of your health.
Enzymatic Therapy for Heel Spurs
 What You Should Know About Treatments like Acid-A-Cal
What You Should Know About Treatments like Acid-A-Cal
It’s common sense that invasive medical procedures like surgery should be a last resort when it comes to treating plantar fasciitis or heel spurs.
But when it comes to evaluating the effectiveness–and safety–of alternative treatments, the internet can be both a wealth of information and an overwhelming slog through information that’s difficult to evaluate.
Enzymatic therapy to treat heel spurs, including the popular brand Acid-A-CalTM, is one of the latest popular alternative treatments for heel spurs. But how does it work? Is it worth the hype? What are the pros and cons for this new type of therapy?
Keep reading to find out!
Are Herbal Remedies for Heel Spurs Effective?
It’s worth noting that heel spurs and plantar fasciitis don’t develop in isolation. While the symptoms are localized to the heels and arch, these symptoms develop in reaction to processes throughout your entire body. Weight gain, improper gait, intense physical activity, and so forth can trickle down to problems in your feet and heels.
In other words, it only makes sense that herbal remedies such as enzymatic therapy, which influence how calcium is absorbed in your body, could be a potentially method for treating heel spurs.
How does Enzymatic Therapy Work?

Enzymatic therapy, in the form of herbal supplements like Acid-A-Cal, works to help your body absorb calcium more easily by regulating your body’s pH. The theory behind this treatment is that high alkalinity can make it far more difficult for your body to absorb calcium.
How does this help with heel spurs? Poor calcium absorption (which can occur even if you are taking calcium supplements, depending on your body’s pH and your ability to absorb it), can lead to brittle, porous, and weak bones–as well as heel spurs. Proper calcium absorption, along with silica and magnesium, can help your bones absorb calcium. This can also reduce the presence of heel spurs.
Pros of Enzymatic Therapy for Heel Spurs
There’s certainly plenty of anecdotal evidence advocating for enzymatic therapy treatments like Acid-A-Cal! A quick scan of reviews on Amazon.com will yield many positive reviews.
It’s important to remember that despite these excited reviewers, there isn’t conclusive evidence yet about how effective this therapy is. However, as far as potential benefits are concerned, enzymatic therapy has several:
First and foremost, enzymatic therapy is created to help people with calcium absorption problems (which can lead to the presence of worsening of heel spurs, with or without plantar fasciitis). Heel spurs can be made worse when the bones are weak and porous because of calcium deficiency. And by strengthening your bones through better calcium absorption, many people have found that their heel spurs improve as well.
Enzymatic therapies like Acid-A-Cal also aim to improve the pH-balance of your digestive system, which not only improves your ability to absorb calcium but improves your absorption of other critical nutrients like magnesium and B-12. Enzymatic therapy can also help stave off osteoporosis.
Cons of Enzymatic Therapy for Heel Spurs
While enzymatic therapy may be helpful for some individuals with heel spurs, it isn’t likely to be helpful for everyone with heel spurs.
Why?
For two reasons. First, this type of therapy is only made to be helpful if you have a calcium absorption problem caused by an overly alkaline pH.
Second, heel spurs typically develop in response to plantar fasciitis, as the body’s response to a compromised and damaged arch. Without addressing the underlying problem of plantar fasciitis through orthotic inserts, rest, icing, and stretching, your heel pain will continue and likely get worse.
Other cons of using enzymatic therapy, including Acid-A-Cal, is the fact that many contain ammonium chloride. This is the same ingredient found on cough syrup and can lead to complications such as kidney stones or acidosis in diabetics.
Is Enzymatic Therapy Right for You?
The decision of whether enzymatic therapy is right for you should be made with your doctor, and after careful research. It’s important to note that it’s very possible to improve your calcium absorption and increase your intake of helpful supplements like magnesium, without adding some of the potentially dangerous ingredients contained in some enzymatic therapies (such as ammonium chloride). All of these supplements can be purchased separately, over the counter.
Talk to your doctor about whether enzymatic therapy is right for you, and how much, if any, supplements you should be taking for strong bones.
And remember, if you have heel spurs as a result of plantar fasciitis, it’s important to treat the underlying disorder–not just the symptoms (aka, heel spurs!). Specialized orthotic inserts have been proven to be 90% effective in treating plantar fasciitis, and position the arch so that the pain from heel spurs is drastically reduced or eliminated. Rest, icing, and stretching exercises are all tried and proven ways to improve the underlying condition of plantar fasciitis as well!
Have a Bump on Your Heel? Here’s What You Should Know
Have you discovered a lump on your heel? If so, you probably have plenty of questions and more than a little concern. What does this new lump mean? What caused it to appear there in the first place? Is it serious? And how can you make it go away?
While finding a lump on your heel can be very concerning, the first thing you should know is that lumps on the back or bottom of your heel aren’t usually a sign of a serious underlying condition, despite the fact that they can be painful. And most can be treated at home, with non-invasive, natural methods.
Let’s take a look at the symptoms, causes, and treatments associated with a lump on your heel.
Symptoms
Symptoms depend a great deal on the cause of the lump itself.
The lump on your heel might show up in either one or both heels. You may notice redness and swelling around the lump, and the lump may be tender to the touch. Lumps may appear on the sides, back, or bottom of the heel.
In most cases, pain you experience from the lump on your heel will get worse if you rise up on your toes.
Causes
There are several conditions that can cause a lump to appear on your heel. Identifying which one you’re dealing with is helpful in determining how to treat the lump, and prevent it from returning!
Haglund’s Deformity or “Pump Bump”
Haglund’s Deformity is also known as “pump bump” because of its primary cause: wearing shoes with a tight heel, like men’s dress shoes or women’s pumps.

The bump develops as the bony section of your heel (which is connected to your Achilles tendon) is irritated and rubbed by ill-fitting shoes causing the tissue of the heel to become irritated. This condition can quickly lead to bursitis, another common cause of heel bumps (read more below!)
People with high arches are particularly at risk for Haglund’s Deformity, since their gait puts extra pressure on the outside of their heel.
-
 High Arch Sole Seats$39.95
High Arch Sole Seats$39.95 -
 GEL Heel Seats (Pair)$24.95
GEL Heel Seats (Pair)$24.95 -
 HTP Heel Seats (Pair)$24.95
HTP Heel Seats (Pair)$24.95
Bursitis of the Heel
Bursas are fluid-filled sacs located at the joints in your body. Retrocalcaneal bursitis, or swelling of the heel bursa (located where your Achilles tendon connects your calf to your heel bone), in response to overuse or irritation, can cause a painful lump to appear as the bursa becomes inflamed.
Haglund’s Deformity, caused by irritation to the heel bone, can quickly cause bursitis if left unaddressed. Other causes of bursitis include repetitive motions that involve the feet and heels, such as running and jumping.
Retrocalcaneal bursitis can sometimes be mistaken for Achilles tendonitis, because of the location of the bursa on the heel. A painful lump can often be a distinguishing characteristic.
If not treated promptly with rest, anti-inflammatories such as ibuprofen, and greater support to the heel and foot, bursitis can become chronic and require more invasive and costly treatment.
Plantar Fibroma
If the lump on your heel develops gradually, appears on the bottom of your foot, and is less than an inch in diameter, it may be a plantar fibroma–a benign lump that is a mass of cells.
Plantar fibromas usually show up on the bottom of your foot, beneath the heel. Wearing shoes, or putting pressure on the fibroma may cause pain. There’s some debate as to the cause of fibromas, but most doctors believe there is a genetic component.
Soft-Tissue Masses
While most other lumps on the heel or foot are simply cysts, a benign soft-tissue mass that is not painful to the touch, a few conditions that present as a lump on the heel may be more serious. Synovial Sarcomas, which are malignant, can also show up as a lump on the foot or heel, and are typically small, firm, and painless.
If you have experienced previous trauma to the foot through an accident, in which an object penetrated your foot, you may develop a mass caused by a foreign body reaction.
When in doubt, consult your doctor!
Treatments
Whether the lump on your heel is caused by Haglund’s Deformity, Bursitis, or a Plantar Fibroma, the recommended treatments are similar. If inflammation is present, icing and the use of non-steroidal anti-inflammatory drugs like ibuprofen or aspirin can help reduce redness and discomfort.

Rest is also an important treatment; try to stay off your feet when possible, and give your feet breaks throughout the day. If repetitive exercise or motion is the culprit, you may need to do more cross-training or change your exercise regimen.
If shoes are the cause of the irritation, wearing comfortable shoes with a less restrictive heel or an open back for a period of time can reduce irritation to the heel bone and bursa.
Specialized orthotic inserts for plantar fasciitis can also provide a great deal of relief, particularly if the bump is on the bottom of the heel, by realigning the foot and reducing pressure on the lump.
Special stretches that help strengthen the tendons and ligaments of the feet and heel can also improve the underlying conditions that are causing the lump on your foot to appear, by giving your foot and heel more support and flexibility.
Your doctor may also recommend an ultrasound or MRI to ensure a correct diagnosis of the lump on your foot.
If the lump on your heel doesn’t respond to the treatments listed here or gets worse, it’s never a bad idea to consult with a medical professional. But for the most part, lumps that appear on the back or bottom of your heels can be treated at home and will go away on their own with a little time and attention–particularly if you begin treatment quickly!