The Plantar Fasciitis Sandal Guide
 A diagnosis of plantar fasciitis doesn’t have to go hand in hand with a pair of boring, expensive heavy orthotic shoes. With light, reusable orthotics inserts, almost any pair of shoes can be transformed into a plantar-fasciitis-fighting machine!
A diagnosis of plantar fasciitis doesn’t have to go hand in hand with a pair of boring, expensive heavy orthotic shoes. With light, reusable orthotics inserts, almost any pair of shoes can be transformed into a plantar-fasciitis-fighting machine!
But what about when summertime rolls around, and those toes need some sunlight?
We think your pedicure deserves to be seen too.
Which is why we’re exploring your options for sandals that are compatible with healing from plantar fasciitis.
Click here to get the only sandals that target heel pain!
Can I Really Wear Sandals If I Have Heel Pain?
The short answer? Absolutely yes!
The longer answer? You need to find the right sandal. Cost, effectiveness at healing plantar fasciitis, and style are top considerations when it comes to summertime, sandals, and plantar fasciitis.

The Best Sandals for Plantar Fasciitis
Specialty Supportive Sandals
Specialty sandals provide more support and cushioning than the average sandal, but aren’t specifically made to treat plantar fasciitis.
Cost: The cost for specialty supportive sandals is higher than your average, running between $40 and $100 for a good pair (of course, the sky’s the limit when it comes to shoes!)
Effectiveness: For max effectiveness, look for sandals that have a thick, cushioned sole, at least some arch support (read: not pancake flat!) and straps that keep your foot from sliding around while you walk. While these sandals won’t do much to heal your plantar fasciitis, they are much less likely to exacerbate or cause the condition.
Style: Birkenstocks are the classic supportive sandals–wide straps, thick soles, and support for your heels. However, many manufacturers and brands make more supportive sandals now, so style options are growing!

Orthopedic Sandals
Orthopedic sandals are made especially to support plantar fasciitis:
Cost: The cost for most orthotic sandals can be pretty steep and will set you back between $100 and $150 per pair. Luckily, you can get sandals with Fascia Bar Technology for only $54.95.
Effectiveness: Heel Seat Sandals are guaranteed to reduce pain from plantar fasciitis and heel spurs. However on the lower end, sandals branded as “orthopedic” are simply a cushioned, supportive sandal. Higher end orthopedic sandals help with heel and foot alignment to reduce the pressure on the plantar fascia while adding cushioning and support for painful feet.
Style: While there are more styles available than ever, the world of orthopedic sandals is still quite limited. It may be difficult to find a pair of orthopedic sandals that fit your unique style.
Regular Sandals With Heel Seat Wraps
Heel Seat Wraps are neoprene, lightweight wraps that are specifically made for healing plantar fasciitis. They can be worn with virtually any type of footwear–including sandals!

Photo shared by customer Kristi D.
Cost: A pair of heel wraps are $34.95 and can be easily washed and reused. Best of all they can be worn with your favorite pair of sandals.
Effectiveness: Heel Wraps turn almost any pair of sandals into orthopedic footwear that’s both lightweight and inexpensive. Fascia-Bar Technology supports your feet and allows you to free your toes while supporting your heels.
Style: Style options are essentially limitless with Heel Wraps. Wear them with your favorite pair of sandals, or even wear them barefoot (the non-slip neoprene means that you can wear these handy wraps even on slick hardwood.)
Are your feet feeling happy yet? Make this the best summer yet by giving your toes a chance to enjoy those summer nights as much as you do this year–and in style to boot (no boot needed!)
Pros & Cons of Heel Pain Surgery

Approximately 95% of plantar fasciitis cases can be successfully treated without surgery. However, for the remaining 5% of cases that do not respond to more conservative treatment methods (like icing, stretches, orthotic inserts, and rest), surgery may be recommended by your doctor.
As with any major medical procedure, the decision to undergo surgery should be made after very careful consideration, and in collaboration with your doctor. At the end of the day, the very best advocate for your health is you!
Thorough research, as well as a hard look at the pros and cons of using surgery to treat heel spurs and plantar fasciitis, is the best way to ensure that you are making an informed decision–and the best decision for your health.
Let’s take a look at the pros and cons involved in surgery for plantar fasciitis.

Pros of Heel Pain Surgery
There are two major pros when it comes to plantar fasciitis surgery: options and success rate. If more conservative treatment methods have been exhausted, don’t despair! In the 5% of plantar fasciitis cases that don’t respond to other types of treatment, surgery offers new options and a high success rate.
Options for Severe Cases of Plantar Fasciitis
It’s a hopeless feeling to be out of options. And if treating plantar fasciitis using conservative treatment methods hasn’t eliminated or drastically reduced your pain level, it can be both frustrating and demoralizing. Thankfully, surgery provides options for these severe cases to successfully treat heel pain from plantar fasciitis.
Most experts agree that conservative methods of treatment should be consistently employed over the course of nine to twelve months–particularly the use of orthotics and exercises designed to treat plantar fasciitis. Before undergoing surgery, make sure to research your options thoroughly and understand all of the cons (see below!) associated with surgery.
High Success Rate
Plantar fasciitis surgery has lasting results and high success rates for most people who undergo the procedure. One study, conducted in 1993 by the Podiatry Hospital of Pittsburgh, found that 39 out of 40 patients who underwent surgery for plantar fasciitis, would recommend the same decision to others, even five years later.

Some methods are considered more effective than others within the medical and podiatric community, so be sure to discuss your options with your doctor, and recognize that there is not a “one size fits all” solution when it comes to surgery. Endoscopic surgery, in which a small camera is inserted through slits in the heel so that the surgeon can see and remove the injured portion of the plantar fascia, is often the first choice for doctors. However, it’s not the only choice. Ask questions about how much of the plantar fascia will be removed, whether any heel spurs will be removed, and why. The answers to these questions will help you understand why a particular procedure has been recommended for your unique case.
Cons of Heel Pain Surgery
As with any major medical procedure, surgery for plantar fasciitis and heel pain shouldn’t be taken lightly because of a few significant risks and potential complications. By educating yourself to prepare for potential risks and consulting with your doctor, you can make the very best choice for your unique situation.
Cost
The cost of plantar fasciitis surgery varies by your location, the type of insurance you have, and the specifics of your unique situation and medical case. But in general, costs are steep, and can easily reach upwards of $10,000.
Recovery Time

Recovery time can be a serious con, since it may be six to 10 weeks before you are able to comfortably walk around without assistance, and three months before you’re able to resume more rigorous activity and exercise.
Depending on the type of surgery you elect, it may also be necessary to wear a cast or brace for several weeks to allow the tissue to heal. Depending on your job, family demands, and other considerations, this can be a serious consideration.
Risks and Complications of Heel Pain Surgery
While a full recovery is always the hope when it comes to surgery, and success rates are high, the potential risks and complications of plantar fasciitis surgery are real. Possible complications and risks include post-surgery infections if the wound is not properly cleaned and cared for. There is also the risk of arch reduction, meaning that it’s less able to bear impact and weight without injury even after healing from surgery.
Some patients report feeling numbness as a result of nerve damage during surgery, and a small percentage of patients find that surgery does not reduce or eliminate their heel pain. still recovery following plantar fascia surgery. It’s very important to discuss these risks with your orthopedic surgeon to decide if the procedure is right for you.
Alternative Treatments

Given the risks, cost, and potential complications of plantar fasciitis surgery, most doctors recommend trying more conservative methods consistently for one year prior to electing surgery. Before you decide to undergo surgery, use the following natural treatment methods consistently:
- Religiously rest your feet twice a day for twenty minutes. While resting your feet, apply an ice pack to reduce inflammation. This can be extremely difficult for busy people, but rest is absolutely critical to healing!
- Commit to daily plantar fascia and heel stretching exercises. It might be hard to believe, but simple stretches designed specifically for plantar fasciitis can really reduce morning heel pain and daily heel pain and to promote eventual recovery.
- Commit to wearing specialized orthotic shoe inserts, every day, in all of your shoes. In more than than 9 out of 10 cases, Fascia-Bar technology has been shown to heal plantar fasciitis by realigning the injured plantar fascia ligament and cushioning the heel.
In rare cases that do not respond to the above natural treatments, your doctor may also recommend medications and cortisone injections as short-term aides.
No one wants to undergo surgery, but by exhausting natural options for healing, educating yourself about pros and cons, and consulting with your doctor to find the right method of treatment for your unique case, you’ll be ready to take advantage of the best option for you!
Commonly asked questions about heel pain surgery
In one study, 97.5% of patients who had heel pain surgery were happy with the procedure.
The cost of heel pain surgery will depend largely on how good your insurance coverage is. Without insurance, it ranges from $10,000 and up. If your insurance covers 90% of the surgery costs, that means you will be responsible for $1,000 or more.
Recovery time depends on the exact type and method of the procedure you and your surgeon choose. It normally takes 6-10 weeks before you are able to fully bear weight on your foot and walk without assistance, and 3-6 months before you can get back to your regular exercise routine and activities.
Plantar fasciitis surgery can be deemed necessary by your medical team, so most insurances will cover at least part of the cost of plantar fasciitis surgery. Be sure to look into your exact insurance plan: some require you to meet a deductible before they cover any expenses, and others will hold you responsible for a coinsurance percentage. Make sure you call your insurance company prior to your surgery and double-check that the facility and doctors you chose are in-network.
What is Foot Drop?
 Imagine, for a moment, walking with one foot inside an inflexible boot.
Imagine, for a moment, walking with one foot inside an inflexible boot.
That classic, step-slap sound resulting from the inflexible boot hitting the ground with each step, is also the hallmark of foot drop, a gait abnormality that is the result of muscle weakness, nerve damage, or partial muscle paralysis to either one or both feet.
Individuals with foot drop are no longer able to properly flex one or both foot, resulting in a “slap” to the ground with each step, rather than a smooth, rolling step from heel to toe.
Foot drop can also cause what’s known as “steppage gait,” in which the affected foot is lifted much higher than normal while walking. Due to the foot’s inability to flex and lift like normal, the toes often drag while the affected leg swings forward. To compensate, this leg must be lifted higher than normal to avoid tripping over the dragging toes.
What are the causes of foot drop, how is it diagnosed, is it permanent, how can it be treated, and should surgery be considered?
Causes of Foot Drop
The causes of foot drop vary significantly, and the prognosis for recovery depends a great deal on the cause itself. Foot drop can result from weakness in the muscles of the legs and thighs, to much more serious conditions like multiple sclerosis. Foot drop can be caused by any of the following:
- Herniated disks in the back that compress and damage nerves leading down to the feet
- Injuries to the pelvis and the hips
- Dislocation of the knees (it’s important to check for nerve damage and artery damage if you ever dislocate your knee!)
- Inadequate blood supply (also known as ischemia). This can take place during a stroke
- Injuries to the sciatic nerve
- Partial paralysis of muscles in the legs
- Muscle weakness or damage
- More serious degenerative conditions like multiple sclerosis, ALS, and cerebral palsy
- Spinal cord injuries
- Exposure to toxins that have damaged the nerves
Diagnosing Foot Drop
Foot drop can often be diagnosed simply by hearing the cadence of your gait on a hard surface. The “slap gait” is distinctive, as one foot or both hit the ground with a slap. In a typical gait, the heel strikes the ground first, followed by the rest of the foot in a controlled and smooth motion. In cases of drop foot, the ability to control the foot’s smooth descent to the ground is absent–the reason for the characteristic slap. Evidence of “steppage gait,” where the affected foot is raised higher than normal to avoid dragging or tripping on the toes, is also a hallmark.
Foot drop can also be diagnosed through examination of dorsiflexion, or the amount of control over your ability to lift and flex downward and upward. The inability to flex the foot with a proper range of motion means that the foot cannot facilitate a normal gait.
Is Foot Drop Permanent?
Foot drop can either be temporary or permanent, depending on how much damage has been sustained, how long it has been happening, and the cause of the muscle or nerve damage to begin with. If you notice foot drop, it’s critical to address the problem and determine the cause as soon as possible.
Treatments for Foot Drop

The main factor in deciding how to treat foot drop is the cause. Some treatments, depending on the cause of foot drop, may include physical therapy, treating a herniated disc, anti-inflammatory drugs to deal with swelling and inflammation at the source of the damaged muscles or nerve, as well as a specialized exercise program to strengthen and repair damage.
Neuromuscular Electrical Stimulation (NMES) may be recommended by your doctor, depending on the cause and extent of the damage to nerves. This treatment stimulates and helps restore function to damaged nerves is minimally invasive.
While you and your doctor are treating the cause of foot drop with a medical professional, foot orthoses, or orthotics, can be very helpful in stabilizing the foot and ankle, which help keep the foot from dropping or dragging during walking and activity. Orthotic shoes can add additional weight to the foot, exacerbating the symptoms of foot drop, so lightweight slip-in orthotics should be used.
Should I Consider Surgery for Foot Drop?
Surgery should typically be a last resort, and foot drop is no exception. Surgery to remedy foot drop yields mixed results, and all are accompanied by long recoveries and invasive, painful procedures. However, some people have seen improvement after surgery for foot drop after exhausting other options for treatment.
The best way to approach foot drop is to treat the symptoms (by using slip-in orthotics and any other treatments your doctor recommends), and working with your doctor to uncover and treat the root cause. Knowledge is power, and learning as much as you can about this condition while finding the treatment that works best for you is key!
Acupressure vs. Acupuncture for Heel Pain
 Acupressure versus acupuncture–what’s the difference, how does each one work, and which one is more effective for plantar fasciitis?
Acupressure versus acupuncture–what’s the difference, how does each one work, and which one is more effective for plantar fasciitis?
These two words sound alike for a reason. Both are rooted in the prefix “Acu,” which means targeted. And both pinpoint heel pain caused by plantar fasciitis. Acupressure–as you have probably guessed–combats heel pain through targeted pressure to different areas of the heel, while acupuncture treats heel pain through special needles that barely puncture the skin.
Here’s what you need to know about acupuncture and acupressure for heel pain:
How Does Acupuncture Help Heel Pain?
In acupuncture, very tiny needles are quickly inserted shallowly. It’s unclear exactly how this works to reduce pain, but researchers believe that the needle insertion stimulates blood flow and hormones to the affected area, drastically reducing pain. Several studies have shown acupuncture to be an effective method of temporarily reducing the symptoms of heel pain and plantar fasciitis. For example, this study by Dr. Tillu and Dr. Gupta showed that pain was significantly improved after 4 and 6 weeks of acupuncture treatment.
How Does Acupressure Help Heel Pain?

Acupressure works through applying pressure to “hot spots” of the heel and arch that have been negatively affected by plantar fasciitis. This accomplishes two things: first, the pressure to these targeted areas numbs the body’s pain response. Second, constant, targeted pressure through special orthotic inserts that incorporate Fascia-Bar technology lifts the arch so that heel spurs no longer dig into the fatty pad of the heel (a primary cause of pain from plantar fasciitis.)
Benefits and Drawbacks of Acupuncture for Plantar Fasciitis
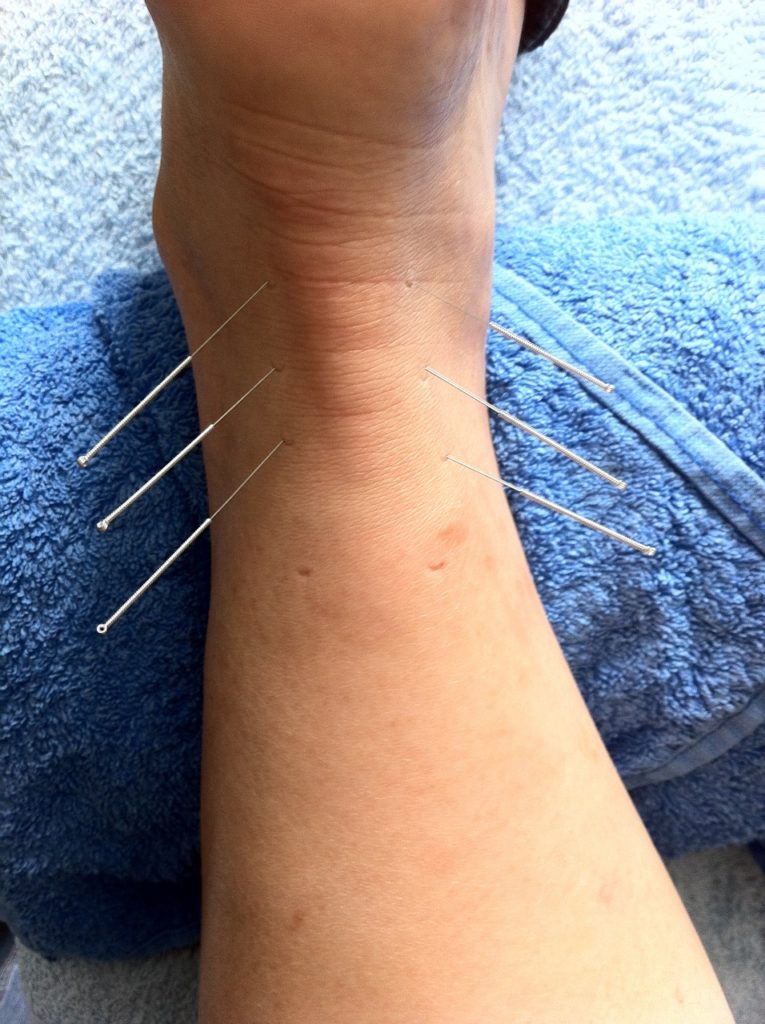
Most of the potential drawbacks to acupuncture for heel pain involve overcoming the perception that acupuncture is painful. While this treatment method does involve needles, it really doesn’t hurt! The other potential downside of acupuncture is that it only treats symptoms–not the cause–of plantar fasciitis. To eliminate symptoms for good, it’s necessary to treat the damage to the plantar fascia.
- Effectiveness: A compelling number of studies indicate that acupuncture is very effective at treating the symptoms of plantar fasciitis. However, acupuncture does not treat the root cause of plantar fasciitis.
- Cost: The cost of acupuncture varies by location and facility, but as a general rule, an intake visit will cost somewhere in the neighborhood of $75, while an ongoing series of visits will be closer to $50.
- Pain Level: Surprisingly, acupuncture isn’t painful. If you do experience pain or discomfort, let the physician know immediately!
Benefits and Drawbacks of Acupressure for Plantar Fasciitis
The biggest drawback to acupressure is finding an orthotic that fits the bill. Most orthotics provide cushioning–important for painful heels–but that’s the end of the story. For effective acupressure, it’s critical to use an orthotic that uses Fascia-Bar technology, which was developed specifically to treat plantar fasciitis and heel spurs. Unlike many treatments for plantar fasciitis (including acupuncture), acupressure focuses on treating the root cause of plantar fasciitis by lifting the plantar fascia to a proper height. This both eliminates the pain from heel spurs, and applies pain-relieving pressure to targeted areas.
- Effectiveness: A double blind clinical study conducted by the University of Iowa concluded that Fascia-Bar technology is twice times as effective at treating heel pain than comparable leading brand orthotics. Patients who use orthotics with Fascia-Bar technology report a remarkable satisfaction rate of more than 90%.
- Cost: Orthotics with Fascia-Bar technology can be purchased for less than $20, and can be washed and reworn.
- Pain Level: While it’s recommended that you ease into wearing orthotics by gradually increasing the amount of time you spend wearing them each day, you shouldn’t experience any pain.
So, Is Acupressure or Acupuncture Better for Heel Pain?
Both acupressure and acupuncture have compelling benefits, and the good news is that you don’t have to choose! These treatments can be used in tandem to provide pain relief from symptoms, depending on your budget and preferences.
While it’s important to treat the root cause of plantar fasciitis to avoid an endless loop of treating symptoms without addressing the underlying issue, any reasonably priced, safe, non-invasive treatment that effectively alleviates pain is a good option!
Benefits of Yoga for Heel Pain (+5 Poses You’ll Love!)
 You’ve probably heard about the many health benefits of yoga by now–including flexibility, strength, and mental clarity.
You’ve probably heard about the many health benefits of yoga by now–including flexibility, strength, and mental clarity.
But did you know that yoga is also a great way to treat foot pain, including plantar fasciitis?
Yoga, which is a fusion of stretching, exercise, and mental awareness, is one of the oldest known forms of exercise and can be an excellent way to relieve heel pain, strengthen and stretch the foot muscles, and provide healthy low-impact exercise for people who suffer from plantar fasciitis.
Keep reading to learn about the benefits of yoga for plantar fasciitis, the best yoga stretches for heel pain, and how to maximize yoga for heel pain.
Benefits of Yoga for Plantar Fasciitis
Plantar fasciitis and yoga are a perfect match for a number of reasons:
Get in Touch With Your Body
Two of the most critical tenets of yoga include getting in tune with your body and strengthening your body–which are both great ways to approach plantar fasciitis! Recognizing when your body needs to rest as you exercise or go about your life is one of the biggest keys to avoiding and healing plantar fasciitis, since many instances of the condition are caused when the body has been pushed too far–leading to tearing or inflammation.
Improve Your Strength and Flexibility
Yoga centers heavily on stretching–which is one of the most effective ways to heal and strengthen damaged fascia! Stretching and strengthening the plantar fascia allows your arch to support weight and impact more effectively, reducing the likelihood of injury and allowing the different ligaments, muscles, and tendons in the feet and legs to support each other more effectively.
Improve Your Pain Without Expensive Medical Bills
Another benefit of doing yoga for heel pain is that the stretches and poses can be done from the comfort of your own home. An incredible 90% of plantar fasciitis cases can be healed without painful and invasive surgeries, procedures and medication. If you want to see even faster results at home, use yoga in combination with other natural remedies for plantar fasciitis to put your feet back on the path to healing faster than you can say “Bandhakonasana.”
Click here to get natural and 100% guaranteed heel pain inserts.
Best Yoga Stretches for Improving Plantar Fasciitis
As a general rule of thumb, you’ll want to stick with low impact stretches (most are!) and avoid stretches that put a lot of pressure on your arch or heels, or that require sudden movements.
Standing poses, poses that stretch calves and Achilles tendon, and poses that gently stretch the arches of your feet are ideal. The following are five of the very best yoga stretches for plantar fasciitis:
1. Toes Pose
This pose, found in Yin Yoga, targets the fascia of the body to stretch, strengthen, and elongate it.
To do Toes Pose, sit in a kneeling position. Then slowly lift up on your toes, with your knees still anchored in front of you on the ground. Gently let your weight settle back onto your heels, and hold this pose for between two and three minutes. Don’t get discouraged if this is difficult at first, or if you can’t hold the pose for this long. As you do this pose, imagine your fascia elongating and becoming more flexible. Don’t forget to breathe calmly and deeply through this pose.
2. Garland Pose
Garland pose stretches the ankles and calves for increased flexibility and strength in critical muscles that support your arch.
To do Garland pose, squat on the floor with your heels flat on the ground and your feet close together and your thighs apart. As you exhale, lean forward so that your torso fits between your thighs. Now, bring your hands together as you gently press your elbows against your inner knees. Hold this position for 30 seconds, then slowly release.
3. Tadasana (Mountain Pose)
Standing poses like this one are a great way to strengthen your legs and feet, stretch the fascia, and relax your body.
To do Tadasana, stand upright with your feet parallel and your big toes just barely touching. Lift the balls of your feet gently, then lower them back down. Rock your body side to side, then back and forth, finally coming to a standstill with your weight balanced across both feet.

4. Baddha Konasana (Bound Angle Pose)
This pose is great for people whose feet are fatigued and strained from spending a lot of time standing. Along with stretching the feet, it stretches the hips, thighs, and calves.
To do Bound Angle Pose, sit down and straighten your back. Then, bend your knees and bring them toward your pelvis until the soles of your feet touch. For support, you can hold your feet with your hands. Use your hands to pull your feet into your body as much as possible, then gently press your knees downward toward the floor. Hold for 1-3 minutes, release, and repeat. As you become more accustomed to this pose, you can increase the difficulty by slowly flapping your knees up and down, like a butterfly.
5. Prancing Feet Pose
This pose is great for building flexibility and strength in your fascia and toes.
To do Prancing Feet Pose, assume a basic standing position. Now, smoothly lift one heel off the ground and roll onto your toes. Place that foot back on the ground and repeat the motion with the opposite foot. Continue alternating sides in a fluid prancing motion. If you feel off balance, hold onto a table or back of a chair while you do Prancing Feet Pose.
How To Maximize Yoga for Heel and Foot Pain
Unlike aerobic exercises, which can put a great deal of strain and impact on your body (think of running, as a main example), yoga offers a low-impact way to stay in shape while improving your strength and flexibility.
If you suffer from heel pain, foot pain, or plantar fasciitis, keep the following tips in mind to maximize the experience for your needs!
Try a Yoga Class
While yoga does exist at a beginner’s level, it typically requires some fundamental knowledge about breathing, poses, and overall control of your body. As a result, we’d recommend starting with a yoga class, or a series of yoga classes. This will help you get acquainted with how yoga works, which will ultimately lead to maximum effectiveness for you.
Tell Your Instructor About Your Heel Pain
Don’t be afraid to let your teacher know that you suffer from plantar fasciitis or another form of heel pain if you decide to join a class! He or she will be able to help you know which exercises may be the most helpful, and which ones you should modify or avoid (like high-impact poses, or sudden pose changes).
Listen to Your Body
When doing a stretch or pose, don’t be afraid to stop if you encounter pain. Let your teacher know, and determine whether you should simply stop the stretch, or in some cases adjust how you’re doing the stretch. While some poses may feel strange at first, you should not feel pain! Listen to your body, and stick to the pace that’s right for you.
Use a Yoga Mat
If at all possible, use a cushioned mat to give your feet the most padding possible and reduce the amount of impact to your plantar fascia. You may want to consider purchasing your own yoga mat to bring with you to class, so you know you’ll have a plush, padded surface!
Choose Yoga Stretches That Focus on Your Feet and Heels
In terms of heel pain, yoga is most effective because of the stretching involved. Yoga stretches help the calf muscles and Achilles tendon remain loose, as well as strengthening the muscles in your feet.
The goal of each stretch in yoga involves releasing energy in the joints of your feet in order to break up scar tissue and adhesions, improve circulation, and increase strength and flexibility. All of this stretching helps with long-term relief from heel pain.
Ready to Give Yoga a Try?
Yoga can be a terrific way to treat your foot and heel pain, but remember that healing takes time. Regularly stretching and strengthening your plantar fascia will promote healing and will strengthen the surrounding muscles and ligaments, allowing your arch to better support weight and resist further injury.
Whether you decide to join a class or do yoga stretches in your own home, you can find motivation knowing that 90% of cases of plantar fasciitis can be treated without medical help. In other words, those relaxing mornings of yoga can make a big difference–without a big bill.
Whether you’re new to yoga or rediscovering the benefits of this helpful practice in a whole new light with plantar fasciitis, you’re taking a great step toward healing. Namaste!