Plantar Fasciitis & Inflammation: Your Questions Answered
 Inflammation and plantar fasciitis go hand in hand, that much is clear. But why? And what can be done about it?
Inflammation and plantar fasciitis go hand in hand, that much is clear. But why? And what can be done about it?
We’ve answered your top questions about plantar fasciitis and inflammation to help you arm yourself with knowledge about one of the most common side effects of this painful condition.
Knowledge is power, and the more you know about the source of your pain, the better you can address–and heal–that pain.
1. Why Does Plantar Fasciitis Cause Inflammation?
To put it simply, plantar fasciitis develops in response to strain and stress on the fascia of your foot–otherwise known as the arch, or the area between your heel and the ball of your foot. When strain or damage from injury or overuse happens, tiny tears appear in the fascia that cause inflammation. As the body attempts to compensate for this damage, small calcium deposits often form that dig into the fatty pad of the heel when you walk–causing further inflammation and pain.
2. How Is Inflammation Identified?
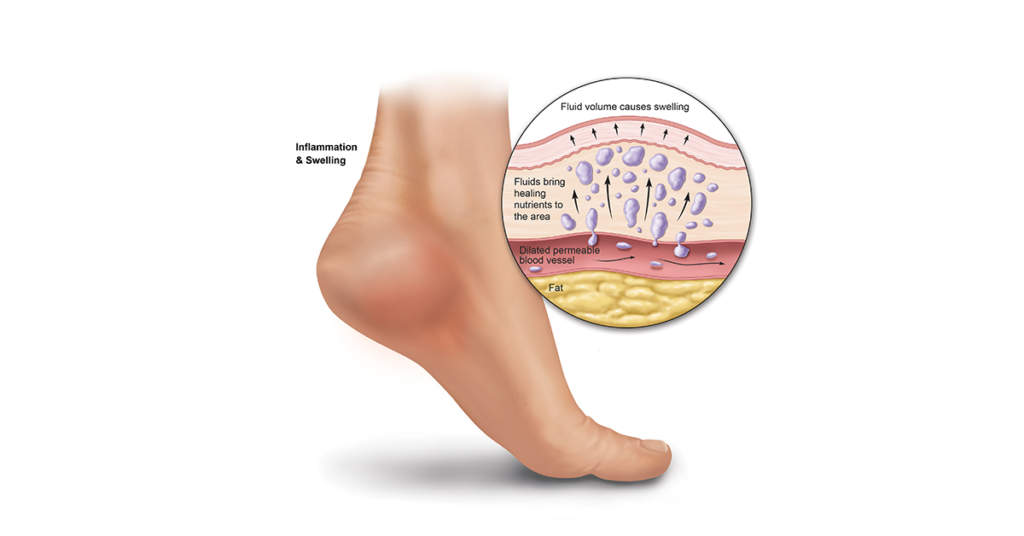
Inflammation typically feels like pain that flares up in the form of swollen tissue, reddened skin, and sometimes heat to the touch. It may feel more difficult to move the inflamed area of the foot. Interestingly enough, inflammation is actually part of your body’s healing response–sending additional blood, hormones, and white blood cells to the injured area of your body for protection and support. It can help to think of inflammation as a signal from your body that something is wrong and needs to be addressed.
3. Can Inflammation Be Present Without Visible Symptoms?
In some cases of chronic, continuous stress and strain to the plantar fascia, it may be possible to ignore or brush off some milder symptoms of inflammation. Pain may not be severe, and redness and swelling may not be apparent to the naked eye at first. Don’t ignore early signs of inflammation like slight swelling and mild pain, before you take action to address the underlying problem.
4. What is the difference between acute and chronic inflammation?
The inflammation you may experience from plantar fasciitis can either be acute or chronic. In other words, the pain you experience long-term as a result of plantar fasciitis is considered chronic, while pain that flares up in the morning when you step out of bed, or when you stay on your feet all day, is acute. Both acute and chronic pain are typically involved with plantar fasciitis, but their treatment should vary.
5. How Can I Treat Acute Inflammation?

Acute inflammation that flares up after a long day on your feet or an injury can be treated with rest, icing, and anti-inflammatory medication like ibuprofen. Make sure to give the injury or the affected area that’s inflamed enough time to heal by staying off your feet as much as possible, and use an ice pack or Ice Slippers consistently over several days.
6. How Can I Treat Chronic Inflammation?
Chronic inflammation should be treated at the source of the problem in addition to using ice, rest, and anti-inflammatory medication for acute symptoms that flare up. Many cases of chronic pain and inflammation of the foot are the result of plantar fasciitis. At the root of the problem is an arch that is injured or strained. By better supporting the arch and positioning the foot so that heel spurs (which can cause inflammation through the simple act of walking as they protrude into the fatty pad of the heel) don’t jut into surrounding tissue, the fascia can begin to heal. Orthotics made especially for heel spurs and plantar fasciitis–not simply cushioning–are the fastest way to heal and support a damaged arch. Incorporating simple stretches to strengthen the arch is also a critical part of healing since a weak arch is much more likely to sustain damage.
When it comes to inflammation, treat the symptoms as they arise, but don’t neglect to treat the underlying problem (typically plantar fasciitis) that is causing the pain and discomfort. Simply treating symptoms is a surefire recipe for a problem that gets worse, and takes longer to treat effectively, as more time goes by. Thankfully, most inflammation resulting from plantar fasciitis can be dealt with simply and effectively at home, using icing, rest, orthotics, and simple stretches.
Vibrating Feeling In Your Foot? It’s Probably Pallesthesia
When it comes to health, nobody likes a mystery.
Which is why a mysterious buzzing or vibrating in your foot that seems to come and go at random is so frustrating.
What Causes Vibrating of the Feet?
This mysterious–and irritating–ailment is the inspiration for numerous questions on Yahoo Answers, online podiatry threads, and doctor’s visits every year. And for many people, the answer for the odd buzzing is “Pallesthesia.”
The buzzing sensation often comes and goes at regular intervals (a few seconds of buzzing followed by a few seconds of peace). It can feel like a short burst of electricity or a cell phone on vibrate under your skin, which is why the name “pallesthesia” literally translates to–”feelings of vibration.”
Often, pallesthesia is most noticeable at night when you’re lying still, trying to fall asleep. It’s also possible to experience it in other extremities like your hands and fingers.
What exactly causes pallesthesia, and should you be worried about other underlying problems?Is there a cure?
Keep reading!
Products to promote healthier feet
Looking to enhance your foot comfort? Give these options a try:
Compression Socks help boost circulation in your legs and can ease swelling and discomfort.
Heel Seats gently realign the tissues of your foot to optimize for health and function.
What Causes Pallesthesia?
To put it briefly, it’s unclear exactly what causes pallesthesia. Or more accurately, there are a number of possible reasons you might be experiencing the vibrating in your foot. The following are some of the most likely possibilities:
B12 deficiency or anemia:
Many people who have suffered from pallesthesia report improvement after upping their dosage of B12 and iron, which makes sense, since these vitamins are key to nerve health, and odd sensations like buzzing could be a sign of deficiency. Check your levels with a simple blood test.
Blocked artery or vein:
Another possibility is a partial blockage in an artery or vein from a clot or some kind of injury. The buzzing sensation may be from the blood forcing its way through the blocked vein or artery.
Stress response and adrenaline:
Does the buzzing feeling in your foot happen when you’re stressed? It may be part of your body’s stress response that sends hormones and blood flow to different parts of the body in anticipation of fight or flight. If you notice that your pallesthesia is happening in response to stress, calming down through breathing exercises or mindfulness can help relieve symptoms.
Compressed nerve or damaged nerve:
Damage to the nerves in the extremities, also known as peripheral neuropathy, can cause pallesthesia in some cases. If you notice any numbness accompanying the vibration, make sure you get to a doctor quickly, since this can indicate damage to the a nerve. Doctors don’t know what causes peripheral neuropathy in many cases. However, about one third are a result of diabetes, which can change blood glucose levels and impact nerve cells’ metabolism.
Medications:
Some medications can cause pallesthesia. If you noticed the buzzing sensation in conjunction with a new medication or increased dosage, talk to your doctor about switching medications, and ask what this means in context of your treatment.
Restless Leg Syndrome:
Some people who suffer from restless leg syndrome, a neurological condition that causes a desire to move one’s legs constantly, report pallesthesia as an accompanying side effect. A good rule of thumb is, if you have other symptoms like pain, fatigue, problems with motor skills, or numbness in addition to the buzzing, it’s worth a trip to the doctor to rule out a larger problem like diabetes, fibromyalgia, arthritis, multiple sclerosis (MS), or a warning of nerve damage.
How Can I Make the Vibrating Go Away?
Because the causes of pallesthesia are so diverse, treatment will depend greatly on the cause of the buzzing.
If you suspect a vitamin deficiency or confirm this with a blood test, increase your B12 or iron, being sure to take care with antacids or calcium that can block absorption of these vitamins.
If you notice a correlation with stress and the buzzing, learn some breathing exercises as a way to calm down when the buzzing starts.
If the underlying cause is more serious, like peripheral neuropathy, diabetes, MS, fibromyalgia, or arthritis, your doctor will be able to coordinate a targeted treatment approach for the underlying condition that should help with the pallesthesia as well.
Can I Prevent Pallesthesia?
As with treatments, preventing pallesthesia rests on its unique cause. In general, work to keep your body healthy through eating lots of whole grains and fruits and vegetables, drink plenty of water, get regular exercise, avoid alcohol and drugs, and avoid repetitive movements that put strain your feet and extremities. Don’t forget a multivitamin, especially one that contains B12 and iron.
The good news is that while pallesthesia is often a mysterious combination of factors, it’s not usually a threat to your health or an indication of something more sinister.
Try the ideas above, and make sure you’re exercising regularly and getting enough vitamins. And don’t hesitate to talk to your doctor to put your mind at ease. Chances are that the buzzing amounts to an annoyance–not a harbinger of bad news. But it’s always better to err on the side of your health.
5 Unexpected Household Items You Can Use to Treat Plantar Fasciitis
 When people hear the words “plantar fasciitis” for the first time–often after months or even years of foot and heel pain–many jump straight to medical intervention.
When people hear the words “plantar fasciitis” for the first time–often after months or even years of foot and heel pain–many jump straight to medical intervention.
But there’s good news for your wallet–and your health. An incredible 90% of plantar fasciitis cases can be resolved without expensive (and sometimes painful or risky) medical intervention.
In fact, many of the most useful tools for treating plantar fasciitis can be found right in your own home.
Check out these surprising home remedies for plantar fasciitis using tools and objects you probably already own!
1. Use a Rolling Pin for Plantar Fasciitis Pain
A simple rolling pin can be a terrific tool for stretching the plantar fascia ligament!
Simply sit in a chair and set the rolling pin on the floor, directly under your bare feet. Then place both feet on the rolling pin and gently roll it back and forth along the bottom of your feet, from the heel to the ball of your foot. Sounds simple, but give it a try–it works!
2. Strengthen Your Feet With a Washcloth
Turns out washcloths are good for more than just cleaning behind your ears.
To do the washcloth stretch, sit on a chair and place a dry washcloth on the floor lying flat, directly in front of your feet. Now, using just your toes, try to pull the washcloth underneath your feet. (Watch this video to see the process).
Sound simple? It is, but it’s also harder than you might think. If you suffer from plantar fasciitis, many of the small muscles in your feet are likely weakened. Over time, as you continue to do stretches, those muscles will get stronger–and your plantar fasciitis will improve! Make sure that with this and other foot exercise you do the stretches evenly. An imbalance in muscle strength in your feet can contribute to an unbalanced gait and uneven weight distribution.
3. Roll Your Feet With A Water Bottle
Take a sip from that water bottle in the fridge. Now, turn it into a great tool to treat plantar fasciitis!
The water bottle stretch is an easy, effective home remedy for plantar fasciitis, heel spurs, and heel pain that relieves tension in your foot muscles and strengthens the plantar fascia. This stretch can also relieve inflammation if you use a frozen water bottle!
Sit in a chair with both feet on the ground and the water bottle lying in front of you on its side. Place one foot onto the water bottle, so that the water bottle is right under the arch of your foot. Now, similar to the rolling pin stretch, slowly roll it back and forth between the heel and ball of your foot 10 times before switching sides.
Lean forward if you’d like to apply more pressure–but never to the point of pain!
4. Use Your Belt to Stretch Your Feet
Make more than a fashion statement with a simple belt. Any color will do–but try to find one that’s wider than one inch for the best results.
This stretch helps relieve tension in and lengthen your calves and feet. Tight calf and foot muscles are a significant contributor to plantar fasciitis, and stretching them can make a big difference in the healing process.
To do the belt stretch, hold one end of the belt in each hand, the put the center of the belt over the ball of one foot. Keep your knee straight while pulling back on the belt (think of this as a reverse arch stretch). Hold for 10 seconds, then relax and repeat, alternating feet, for 10 minutes. You should repeat this exercise twice a day for a week to start seeing results.
5. Use a Thick Book to Stretch Your Calves
Have a couple of thick books? Then you have more than just a good read!
Stack two thick books about two feet away from a wall. Then, stand on top so that just your heels hang off the back edge. Next, carefully lean forward with your hands in front of you (at face or shoulder height) until your weight is supported against the wall in front of you. Hold this pose for 15 seconds, then straighten your back and lift your feet up and down using the balls of your feet. Next, do this stretch with one foot–then switch sides!
Keep in mind that consistency and correct application are the names of the game when it comes to all of these home remedies for plantar fasciitis. Set up a simple schedule to use these tools several times a day, and within a few weeks you should be feeling much better!
As with any treatment, don’t hesitate to consult your doctor if your pain isn’t responding to treatment, or if your pain seems to be getting worse. It could indicate complications or another underlying problem. But for 90 percent of plantar fasciitis sufferers, these unexpected household items can be lifesavers that don’t cost a cent!
Pregnancy and Heel Pain
 Pregnancy can be uncomfortable for a lot of reasons. You’re dealing with morning sickness, weight gain, stretch marks, swollen ankles, and intense cravings (read: Big Mac, hold the pickles, add maraschino cherries.)
Pregnancy can be uncomfortable for a lot of reasons. You’re dealing with morning sickness, weight gain, stretch marks, swollen ankles, and intense cravings (read: Big Mac, hold the pickles, add maraschino cherries.)
And the cherry on top (the one you didn’t request)? Heel pain from plantar fasciitis often develops during pregnancy too.
The good news is, this particular source of discomfort and pain doesn’t have to haunt your entire pregnancy or postpartum days. In this post, we’ll take a look at the reasons you might be experiencing heel pain during or after pregnancy, how to differentiate plantar fasciitis from normal aches and pains, and ways you can reduce or eliminate the pain of plantar fasciitis during pregnancy.
The Connection Between Pregnancy and Heel Pain
As you gain healthy and necessary weight during your pregnancy, the additional strain on the arches of your feet can cause them to flatten. This, in turn, causes your feet to “pronate” or roll inward as you walk, placing a great deal of strain on your plantar fascia ligament.
Pregnancy is strongly linked to the development of plantar fasciitis because weight gain is, necessarily, often more dramatic during this process. The new, rapid increase in strain on your arches causes small rips and tears to appear in the plantar fascia, leading to inflammation, pain, and, if left untreated, “heel spurs” (small, sharp calcium deposits that result from damage to the plantar fascia and dig into the fatty pad of your heel).

Symptoms of Plantar Fasciitis in Pregnancy and Postpartum
It’s normal to experience tired feet now and then–after all, you’re carrying a growing passenger! Normal soreness will usually go away within a day or two. It’s also normal to experience some swelling, especially as your pregnancy nears its conclusion.
It’s important to pay attention to pain that doesn’t subside after a day or so, is worse in the mornings, and is primarily focused on the bottom of your heel. The pain from plantar fasciitis (as opposed to normal aches and pains) will improve somewhat with activity as your ligaments loosen up.
What Can I Do if I’m Pregnant and My Feet Hurt?

Most women anticipate aches and pains throughout pregnancy, but if your feet are aching–especially if your feet hurt but aren’t particularly swollen–it’s important to pay attention to the pain and recognize that plantar fasciitis may be developing.
If you’re postpartum and still experiencing heel pain, plantar fasciitis is a likely culprit as well. If left untreated, heel spurs will continue to be a source of pain and discomfort long after the baby weight is gone.
So, what can you do about plantar fasciitis during pregnancy or postpartum? (As with any form of treatment during pregnancy, be sure to consult your doctor for his or her recommendation and continued medical input!)
- Rest your feet as much as possible. Don’t be afraid to put your feet up and relax, especially during the day. You’ll also want to avoid standing still for long periods of time particularly–since standing is actually harder on your arches than walking!
- Invest in a foot massage. Massage is a great way to reduce pain in the short term, but also can contribute to long-term healing. Ask your partner to rub your feet, try self-massage with a Foot Massage Ball, or splurge on a prenatal massage, preferrably with a massage doula or other pregnancy specialist.
- Avoid high heels at all costs. High heels and plantar fasciitis are strongly linked even without adding pregnancy to the equation. Opt for a pair of cute sneakers or supportive flats that give your toes plenty of room, support your heel and arch, and help you stay balanced. Many women’s feet swell during pregnancy, so don’t be afraid to size up in shoes if needed.
- Give your feet some much-needed support. Orthotic shoe inserts designed specifically for Plantar Fasciitis can be easily slipped into your everyday shoes–and provide badly needed support and relief for your arches. Orthotics that treat plantar fasciitis are shown to have a 90% success rate in drastically reducing or eliminating heel pain.
- Ice your feet regularly. Icing is a terrific way to reduce inflammation and pain from plantar fasciitis. Ask your doctor first to ensure that icing is an appropriate treatment during your pregnancy, then choose one of many inexpensive icing options made just for plantar fasciitis.
- Do simple stretches daily. Stretching is simple, effective–and can be done from the comfort of your own home! Share these free heel stretching videos with your obstetrician to learn which ones are right for you during your pregnancy!
You have a lot on your mind during pregnancy without adding heel pain to the mix. Nip plantar fasciitis in the bud by treating symptoms promptly, and get back to picking out the perfect baby name or whipping that nursery into shape!
Everything You Need to Know About Chilblains
 Chilblains isn’t the easiest word to say (it’s pronounced CHILL-blaynes), but this common condition afflicts millions of people each year when winter weather comes to call.
Chilblains isn’t the easiest word to say (it’s pronounced CHILL-blaynes), but this common condition afflicts millions of people each year when winter weather comes to call.
Also known as pernio or perniosis, chilblains develops when skin–especially in the extremities–is exposed to cold weather. The patches of inflamed skin are often confused with frostbite; however, chilblains is typically more closely related to problems with circulation.
What exactly is chilblains, what are the symptoms, and most importantly, how can it be treated and prevented?
Read on to find out everything you need to know about chilblains!
What Are Chilblains?

Chilblains show up as red, inflamed, painful patches of skin–particularly on the toes, fingers, ears, or nose. The condition is the result of connective damage from cold and humid–but not necessarily freezing–weather. If you notice red patches on your extremities, especially accompanied by itchy and sometimes blistered skin, it’s likely that you have chilblains.
What Causes Chilblains?
Winter weather brings chilblains, that much is certain. But aside from that, it’s something of a mystery why this painful inflammation develops. Failing to protect or properly cover extremities with a hat, gloves, and footwear in cold and humid weather is one of the quickest risk factors in developing the condition–especially if the cold, exposed skin is suddenly exposed to much warmer air afterward.
Some experts believe that when the blood vessels in extremities are rewarmed suddenly, the small blood blood vessels expand more quickly than the large blood vessels, ultimately causing a bottleneck that results in blood leakage into the surrounding tissue.
Risk factors that may predispose individuals to getting chilblains include wearing tight clothing, or clothing that exposes skin to the elements during cold weather. Men are more likely than women to develop the condition, people who are underweight are more at risk than people who are of average weight, and people who live in areas that are not just cold but humid carry higher risk. People with Raynaud’s, diabetes, or other circulatory disorders, are also especially susceptible to chilblains. Smokers are another group that experience higher rates of chilblains.
Symptoms of Chilblains
If you have the following symptoms, you may be experiencing chilblains:
- Red patches of skin, particularly in the toes, fingers, nose, ears, or chin
- Swelling that is accompanied by pain, itching, or a burning sensation
- Blisters sometimes, but not always, accompany chilblains
- Erythema (this means that when you press a finger down on a reddened area of skin, then let go, the area stays white for several seconds)
- Skin discoloration (skin may turn blue or purple in severe cases)
Chilblains may appear and reappear several times throughout the course of a winter, and may even resurface over the course of several years in response to exposure and cold.
The Care and Treatment of Chilblains
The good news is, chilblains usually heal by themselves in 7–14 days. However, you can use the following home remedies to manage the pain caused by the condition. It’s also important to manage chilblains, especially if blisters are present, since these can easily lead to infections.
Home Remedies for Chilblains

- Gently applying moisturizing lotion to the affected areas can help reduce pain and promote healing. Don’t massage or handle the areas roughly.
- Gently apply calamine lotion or witch hazel to affected areas to reduce inflammation and itching
- Protect the affected areas–and all extremities–in cold, humid weather with proper protection, and avoid re-exposing to cold weather.
- When you come inside after spending time in cold weather, allow skin to rewarm gradually. Don’t take off your hat or gloves immediately, but rather allow your skin to acclimate first.
- Keep any areas of skin affected by chilblains clean with antiseptic soap, and resist the urge to scratch.
Medical Intervention
While most cases of chilblains will heal without medical help, keep a close eye on any blistering. If you think your chilblains might be infected, or if you are experiencing high levels of pain, seek medical attention. You also may want to involve a doctor if you have complications like diabetes. Your doctor may prescribe a topical corticosteroid to the affected skin, or blood pressure medicine to help open up affected blood vessels.
Tips for Winter Foot Care
Feet can be especially susceptible to chilblains! And an ounce of prevention is worth a pound of cure. Don’t skimp on the socks–make sure your feet are snug, and that you change wet or sweaty socks quickly to avoid a dangerous combination of humidity and cold.
Keep those feet warm and toasty this winter, and avoid exposure to the elements when at all possible. And if you have any risk factors for chilblains–like diabetes or poor blood circulation–take extra precautions!