What Does Your Toe Length Mean? Top Myths and Facts
According to popular wisdom, your toe length says a lot about you. A quick search of the web will reveal plenty of blog articles about toe length and heritage, toe length and intelligence, and even toe length personality quizzes.
So what’s the real truth about toes?
Does a longer second toe mean you’re dependable? Do long toes mean you’re a quick thinker? Are webbed feet a sign that you’re a party animal?
You’re about to find out! We’re about to mythbust some of the most common perceptions about what your toe length reveals about you!
Myth #1: Your Toe Length Is Indicative of Your Personality
Mostly false. While author Jane Sheehan of Let’s Read Our Feet insists that toe-length is one way to tell a lot about personality, science generally fails to back this perspective. Sheehan says, “It’s all about analysing the structure and texture and imbalances of the feet to understand someone’s emotions and personality.” There may be some truth to the idea that emotions and personality can impact a person’s posture and gait–but the actual length of your toes are determined before birth!
Myth #2: Toe Length Reveals a Person’s Heritage

Mostly false. There’s still some debate as to whether toes that descend perfectly in height are indicative of Egyptian heritage–or whether a tall second toe means you have Greek ancestry. But generally, this notion has been disproven by what we know about genetics. Several studies have shown that toe length is determined by both recessive and dominant genes, the influence of other genes, and environment.
Think of it this way: The combination of dominant and recessive genes play out in much the same way that eye color and hair color do! Relating toe length to ancestry would be like insisting that everyone with brown hair is of American Indian heritage. While that’s true of some people with brown hair, it isn’t true of many others! Toe length is a result of a complicated dance of alleles, genetics, and environment.
Myth #3: Toe Length Correlates with the Length of … Other Body Parts

False! Canadian researchers Jerald Bain and Kerry Siminoski won an IgNoble prize in 1998 for a study of 63 men that proved toe length is simply indicative of, well, toe length.
All in all, the truth about toe length is this: toe length is genetic! And toes come in all shapes and sizes. However, that’s not to say toes aren’t important. Why? Here’s some facts!
Fact #1: Toe Length Can Influence Your Gait
If you have longer than average toes, are missing a toe, or have shorter than average toes, your gait will likely show it to some degree. Diabetes patients who must have one or several toes amputated for the sake of their health are often concerned about their ability to regain a full range of motion while walking or running. However, no matter your toe length, doctors agree that toes aren’t technically required at all for walking or running.
Fact #2: Your Toe Length Should Be Considered When Buying Shoes
Keep your toes in mind when you buy new shoes. Forcing your toes to the front of your shoe if they’re too small, or smushing them downward with high heels that don’t fit well is a recipe for hammer toes, unbalanced gait, and bad posture. Give your toes the room they need, and your feet will thank you for it!
Whether your toes are long, short, or a mix of the two, they’re all yours! Take pride in those toes, and treat them to a pedicure. And don’t forget to take good care of the feet they’re attached to with properly fitting footwear and support for your arches!
21 Surprising Plantar Fasciitis Statistics
 If you or a loved one suffer from plantar fasciitis, you’ve probably heard an earful of surefire remedies, stories about a cousin who was cured after surgery, and a multitude of tips and tricks for relieving pain.
If you or a loved one suffer from plantar fasciitis, you’ve probably heard an earful of surefire remedies, stories about a cousin who was cured after surgery, and a multitude of tips and tricks for relieving pain.
But what do the numbers say when it comes to plantar fasciitis?
We’ve gathered the most compelling–and often surprising–facts about plantar fasciitis from top medical journals and publications. Because when it comes to making decisions about the health of your feet, it’s critical to have the facts on your side!
Top Plantar Fasciitis Statistics
- Right around 10% of people will suffer from plantar fasciitis in their lifetime1.
Takeaway: Plantar fasciitis is pretty darn common! Knowing the facts about this condition can help nip symptoms in the bud.
- A whopping 89% of plantar fasciitis sufferers experience plantar fascia softening2.
Takeaway: Catching plantar fasciitis early is one of the best ways to catch chronic pain at the pass. This makes ultrasound elastography–which can detect plantar fascia softening–an effective diagnostic tool, even in early stages of PF! - In one study, the combination of foot orthosis and an adjustable dorsiflexion night splint resulted in a 47% decrease in pain3.
Takeaway: If just one solution for your plantar fasciitis pain isn’t working, try combining treatments with orthotics and a night splint. - An incredible 85.72% of patients see a decrease in pain with Botulinum type A, or BTX treatments4.
Takeaway: If your symptoms from plantar fasciitis are resistant to home remedies, BTX might be a terrific option. - In one study of 250 participants, orthoses (orthotic inserts) improved pain by 37% after a 12-week period5.
Takeaway: Don’t give up on your orthotic inserts after just a few days! Give it some time, as the best results come from trials of 12 weeks or longer.
- A breakthrough study found that after three months, custom orthoses only improved pain 11% as compared to placebo orthotics6.
Takeaway: Custom orthotics can be incredibly expensive–and might not be worth the extra money! - Plantar fasciitis accounts for between 11-15%7 of all adult foot symptoms requiring the care of a medical professional.
Takeaway: Most cases of plantar fasciitis can be treated effectively with home remedies–however, the remaining cases can be quite stubborn, necessitating medical intervention. - Plantar fasciitis has been reported to account for about 10%7 of injuries that occur in connection with running.
Takeaway: Running is a major culprit for plantar fasciitis injuries. Wearing proper footwear, supporting your feet with orthotics, and resting as needed is key. - Amazingly, 90% of plantar fasciitis cases can be healed with conservative, in-home treatments.
Takeaway: Medical interventions can be costly, risky, and painful. Before jumping to medical intervention, give conservative home remedies a chance. - Heel Seats with Fascia Bar technology are 2x as effective as Dr. Scholls.
Takeaway: Not all orthotics are created equal! Fascia Bar technology is the difference between orthotic shoe inserts that specifically target and heal plantar fasciitis, and inserts that simply provide cushioning. - The annual cost of treatments for plantar fasciitis is estimated to be between $192 and $376 million dollars8.
Takeaway: Medical treatments can get very expensive, very quickly–especially when used as a first resort. Most cases of plantar fasciitis can be resolved at home with conservative, consistent treatment.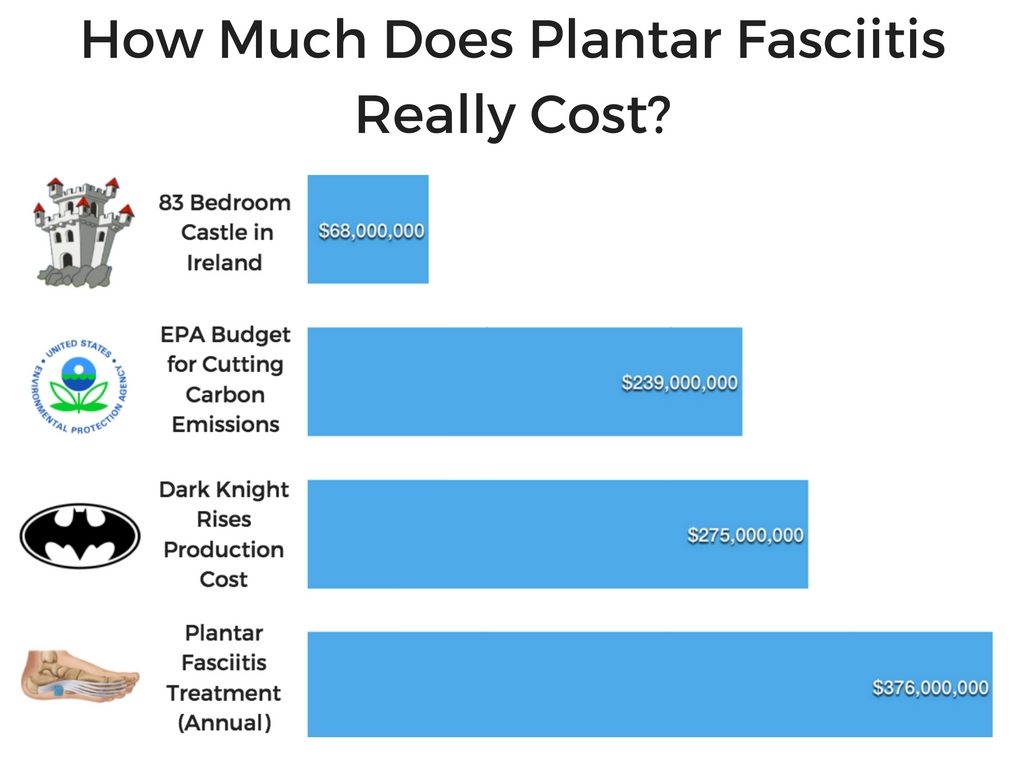
- Obesity is a factor in 70% of plantar fasciitis cases9.
Takeaway: In some cases, gaining weight quickly is a given (pregnancy being the most notable case!) However, in other situations it’s important, if at all possible, to maintain a healthy weight to keep healthy feet. - In one study, heel pain was either eliminated or much improved at eight weeks in 52% of patients7 who were treated with an exercise program to stretch the plantar fascia.
Takeaway: Stretching to relieve symptoms of plantar fasciitis doesn’t work immediately–but it does work in the long-term. Incorporate stretching into your daily routine for best results - Heel Spurs are found in about 50% of plantar fasciitis cases10.
Takeaway: Contrary to common belief, heel spurs are caused by plantar fasciitis–not the other way around! Heel spurs develop in response to trauma of the plantar fascia, which can ultimately cause a great deal of pain when walking. Treating plantar fasciitis early is the key to avoiding heel spurs. - The Centers for Disease Control and Prevention’s National Center for Health Statistics have found that plantar fasciitis accounts for an average of one million patient visits per year.
Takeaway: The pain from plantar fasciitis drives a huge number of people to the doctor’s office annually. That’s no small matter! For many of these cases, symptoms could be resolved with at-home treatments like stretching, icing, and orthotic inserts. - Favorable outcomes were reported in more than 75%7 of patients who underwent surgery in one study.
Takeaway: While surgery should be used as a last resort because of its expense, risks, and the down time involved, it’s a very effective last resort if needed!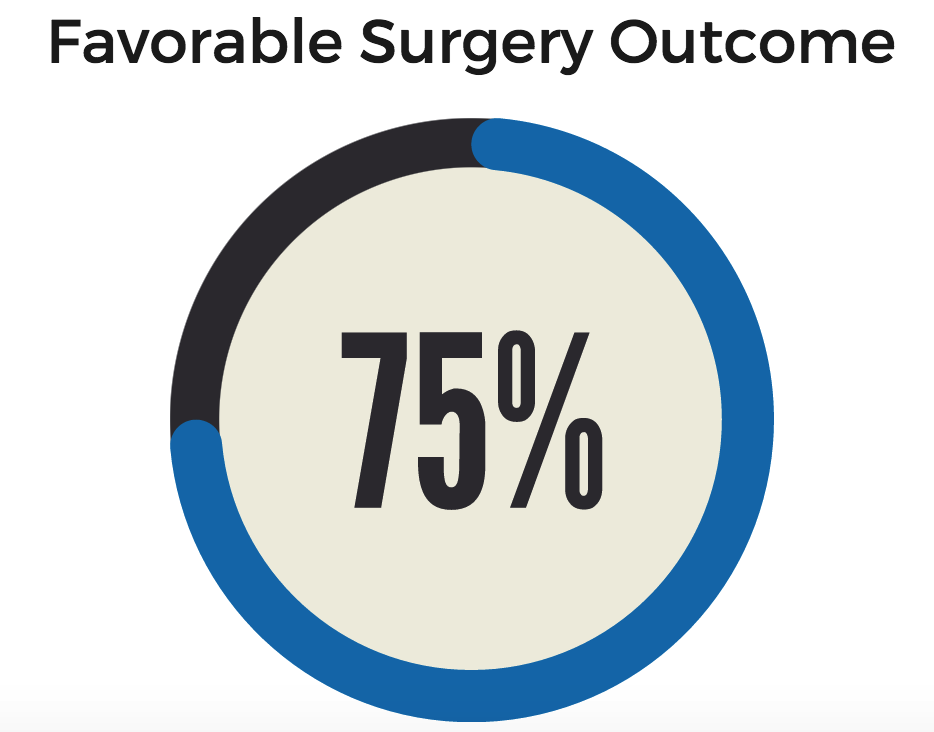
- In one study, 14% of patients noticed an improvement in their plantar fasciitis symptoms simply by wearing more supportive footwear11
Takeaway: Footwear is one of the most important aspects of supporting your heel and arch! Good footwear means better impact absorption, better cushioning, and less heel movement. - Custom orthotics cost between $200-$800 per pair–as compared to the cost of Heel Seats at $24.95 per pair.
Takeaway: Many physicians agree that custom orthotics are overprescribed and very expensive. Heel Seats are much less expensive and have been shown to be effective in 90% of users. - The cost of plantar fasciitis surgery can reach $10,000 or more.
Takeaway: Not only is surgery incredibly expensive, it also involves a lot of physical therapy and down time–and should be a last resort. - In one study, researchers found that 27% of cases of plantar fasciitis had been misdiagnosed.
Takeaway: If your pain isn’t going away, or if insoles and stretching make it worse, you might not have plantar fasciitis. Ligament tears and plantar fibromas are two of the leading conditions that masquerade as plantar fasciitis. - Several studies have shown that use of night splints results in improvement for 80% of patients12. Additional studies find that night splints are especially helpful for individuals whose symptoms have been present for more than 12 months.
Takeaway: Night splints are a terrific option for speeding healing, especially if you aren’t seeing results as quickly as you hoped. Night splints can particularly help with morning pain, one of the hallmarks of plantar fasciitis.
There’s a lot to learn about plantar fasciitis–but the good news is these numbers and statistics paint a hopeful picture. The overwhelming majority of plantar fasciitis cases can be treated effectively–and without costly and painful medical intervention.
The more you know, the more effectively and confidently you can approach your treatment and pain management.
References
- DeMaio, M., Paine, R., Mangine, R. E., & Drez, D. (1993). Plantar fasciitis. Orthopedics, 16(10), 1153-1163.
- Lee, S., Park, H. J., Kwag, H. J., Hong, H., Park, H., Lee, Y., . . . Lee, Y. (2014, September). Ultrasound elastography in the early diagnosis of plantar fasciitis. Clinical Imaging, 38(5), 715-718. doi:10.1016/j.clinimag.2012.12.004
-
Lee, W. C., Wong, W. Y., Kung, E., & Leung, A. K. (2012). Effectiveness of adjustable dorsiflexion night splint in combination with accommodative foot orthosis on plantar fasciitis. The Journal of Rehabilitation Research and Development, 49(10), 1557. doi:10.1682/jrrd.2011.09.0181
- Diaz-Llopis, I. V., Rodriguez-Ruiz, C. M., Mulet-Perry, S., Mondejar-Gomez, F. J., Climent-Barbera, J. M., & Cholbi-Llobel, F. (2011). Randomized controlled study of the efficacy of the injection of botulinum toxin type A versus corticosteroids in chronic plantar fasciitis: Results at one and six months. Clinical Rehabilitation, 26(7), 594-606. doi:10.1177/0269215511426159
- Lee, S. Y., Mckeon, P., & Hertel, J. (2009). Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis. Physical Therapy in Sport, 10(1), 12-18. doi:10.1016/j.ptsp.2008.09.002
- Hawke, F., Burns, J., Radford, J. A., & Toit, V. D. (2008). Custom-made foot orthoses for the treatment of foot pain. Cochrane Database of Systematic Reviews Reviews. doi:10.1002/14651858.cd006801.pub2
- Buchbinder, R. (2004). Plantar Fasciitis. New England Journal of Medicine, 350(21), 2159-2166. doi:10.1056/nejmcp032745
- Young, C. (2012). Plantar Fasciitis. Annals of Internal Medicine,156(1_Part_1). doi:10.7326/0003-4819-156-1-201201030-01001
- Rosenbaum, A. J., Dipreta, J. A., & Misener, D. (2014). Plantar Heel Pain. Medical Clinics of North America, 98(2), 339-352. doi:10.1016/j.mcna.2013.10.009
- Tu, P, & Bytomski. (2011). Diagnosis of Heel Pain. Duke University, Durham, North Carolina Am Fam Physician, 84(8), 909-916.
- Wolgin, M., Cook, C., Graham, C., & Mauldin, D. (1994). Conservative Treatment of Plantar Heel Pain: Long-Term Follow-Up. Foot & Ankle International, 15(3), 97-102. doi:10.1177/107110079401500303
- Young, C., Rutherford, D., & Niedfeldt, M. (2001). Treatment of Plantar Fasciitis. Am Fam Physician. 63(3):467-475.
 |
|
|---|
Plantar Fasciitis and Depression: The Emotional Toll of Plantar Fasciitis
 Plantar fasciitis is a physical condition–but it can also be a deeply emotional experience. Dealing with chronic pain and experiencing discouragement in your efforts to find a solution can be exhausting, frustrating, and infuriating. Studies find that people who suffer from chronic pain are three times more likely to suffer from a mood disorder as well.
Plantar fasciitis is a physical condition–but it can also be a deeply emotional experience. Dealing with chronic pain and experiencing discouragement in your efforts to find a solution can be exhausting, frustrating, and infuriating. Studies find that people who suffer from chronic pain are three times more likely to suffer from a mood disorder as well.
Can plantar fasciitis cause depression and anxiety? Or, can depression and anxiety ever lead to the development of heel pain? In this blog post, we’ll answer some common questions about the connection between mental health and heel pain.
Can Plantar Fasciitis Cause Depression or Anxiety?
It’s not just the toll of navigating chronic pain that links it with mood disorders like depression. Dr. Michael Moskowitz, board member of the American Pain Association, says, “If you look at the nine places in the brain where pain occurs, six of them are where we experience mood disorders like depression and anxiety.” In other words, physical pain and emotional pain are intertwined–literally.
Whether you’re suffering from a combination of chronic pain and depression or anxiety, or are battling higher levels of frustration, hopelessness, and anger, you are not alone. There is help and hope.
Can Anxiety, Depression, or Emotional Stress Cause Plantar Fasciitis?
While depression or anxiety can certainly be byproducts of chronic pain, there’s some evidence suggesting that emotional stress can increase your chances of developing plantar fasciitis.
While heel pain may not be a direct result of emotional distress, it can certainly be a contributing factor for the following reasons:
Increased Oxidative Stress
Oxidative stress— which has been found to be strongly correlated with depression, anxiety, and other types of emotional stress— is also strongly correlated with inflammation in the body. If you’re dealing with high levels of oxidative stress because of depression or anxiety, your plantar fascia may be at increased risk for injury and inflammation.
Changes in Exercise Routine and Diet
If you’re dealing with anxiety, depression, or another type of mental distress you’re likely eating and exercising differently than you might otherwise. Sudden weight gain because of dietary chances can put extra strain on the arches of your feet. Likewise, a sudden increase or decrease in activity level can result in less flexibility of the muscles and tendons in the feet, or extra force and strain that leads to injury.
Coping with Chronic Pain and Depression or Anxiety
If you suspect that your anxiety or depression may be connected to your chronic pain, there are things you can do to care for your emotional wellbeing while you treat your physical pain:
Maintain Self-Care
The mind-body connection is strong. While it’s not always easy to care for yourself physically when you’re not feeling 100% mentally, self-care can make a big difference to your mental and physical health. Make time to rest properly, drink enough water, eat nutritious food, spend some time exercising in whatever way you can, connect with the people you love, and follow your doctor’s recommendations for any medications or treatments you’re trying.
Find Your People
Reaching out and getting involved with a group of individuals who experience the same type of chronic pain you do can be immensely helpful. There are online support groups on Facebook and across the web, or if you prefer face-to-face interaction you can check out meetup.com for local groups, or talk to your local hospital for suggestions and leads. Not only will talking with people in a similar situation help you feel less lonely–it’ll also serve as a great source of new ideas to try, inspiration, friendships, and laughter.
Try Talk Therapy or EMDR
Talk therapy can be a terrific way to work through the emotional angle of dealing with chronic pain. It’s all too easy for sufferers of chronic pain to isolate themselves or withdraw from friends and family, fearing “compassion overload” for an ongoing condition.
Spending time talking with a trained, objective professional can be a great way to work through not only the emotional trauma of chronic pain, but also to help you navigate relationships and relate to friends and family in affirming, helpful ways. Another branch of counseling known as EMDR has also been shown to be particularly effective for targeting the emotional component of chronic pain and trauma. Both talk therapy and EMDR are generally covered by insurance and can provide a tremendous outlet and relief!
Learn About New Developments
It can be hard to try one more new thing–especially when you feel like you’ve tried it all. It can also be hard to get your hopes up, only to feel even more disappointed when a new therapy or treatment doesn’t pan out the way you’d hoped. However, with new technology, you might find that you’re pleasantly surprised by some of the options available–especially when it comes to noninvasive, inexpensive treatment options for plantar fasciitis. Keep your ear to the ground, and pay close attention to volume and quality of reviews before making an emotional (or financial) investment.
Find a Furry Friend
You don’t have to be an animal fanatic to gain the benefits of spending time with our furry friends to help mitigate the emotional toll of chronic pain from conditions like plantar fasciitis. Studies show that spending time with animals reduces levels of cortisol (the stress hormone), as well as levels of anxiety, depression, and pain.
It’s not 100 percent clear exactly why spending time with animals helps so much–maybe it’s their lack of judgment, steady support, or joy at simply being in your presence. If you don’t have a pet, there are many opportunities to volunteer at your local shelter, helping socialize cats, dogs, and other animals.
Write About Your Experiences
Journaling can be a powerful tool in healing when it comes to chronic pain and its emotional toll. The act of expressing yourself and naming your fears, frustrations, and discouragements can help you quantify them, put them in perspective, and explore unexpected feelings. Keeping a journal consistently can also help you more effectively identify and track treatments that work, patterns in your pain and triggers, and strategies for dealing with pain.
Have Some Fun
For many of us, heel pain limits us in our favorite activities. However, having fun is a great way to instantly boost your mood and improve your ability to cope! Try to find new hobbies and activities that do not involve being on your feet – like crossword puzzles, reading, watching funny videos online, or learning a new language.
The connection between chronic pain and emotional distress is real. And caring for your mental health as you navigate the physical pain you experience from conditions like plantar fasciitis is an important part of healing. One step at a time, one day at a time, you can find support and relief for the physical and mental distress you’re experiencing.
Do High Heels Cause Plantar Fasciitis?
 High heels might look fabulous–but looks can be deceiving! There’s a strong connection between wearing high heels and developing plantar fasciitis (not to mention a host of other ailments and problems.)
High heels might look fabulous–but looks can be deceiving! There’s a strong connection between wearing high heels and developing plantar fasciitis (not to mention a host of other ailments and problems.)
So, does that mean your stiletto days are over? Is there a healthy way to wear high heels without sacrificing the health of your heels and feet?
We’ve got your answers!
The Connection Between High Heels and Plantar Fasciitis
The connection between wearing high heels and developing plantar fasciitis revolves around this fact: High heels distribute your weight unevenly and force the arch of your foot into an unnatural position. This impacts your gait as well as the way the force from walking and other activity is distributed–putting a strain on your arch and causing tearing and inflammation.
High heels also typically fail to support your heels with cushioning, meaning that the pad of your heel is pressed into a hard, unsteady surface. And that’s not all. Even not wearing high heels can cause plantar fasciitis (if you wear them regularly enough!) Since high heels leave you with a weakened arch, suddenly switching to more supportive shoes after chronic high heel use still leaves you with an arch that can’t as effectively absorb impact or support your weight.

More Trouble with High Heels
Plantar fasciitis isn’t the only trouble that can come from high heels, unfortunately. Because of the unnatural position of the heel and the raised calf, atrophy of the achilles tendon and a weakened calf muscle can occur. High heels also carry an increased likelihood to injuries of the ankle through a sprain after a fall when the heel catches in a crack or raised surface and the shoe is destabilized, causing the ankle to pitch sideways.
High heels can also harm your toes, which are more compressed because of the downward pressure into the toe of your shoe. Bunions, hammertoes, corns, neuromas, calluses, and ingrown toenails are all common conditions for chronic high heel wearers.
In addition to these problems, wearing high heels can also cause back, neck, and shoulder pain–since high heel’s disrupt the entire body’s alignment as the weight is shifted unnaturally to the balls of the foot.
How to Wear High Heels Without Pain

If you love heels, don’t despair. You can still love your feet without sacrificing the style you love! Simply follow a few key guidelines.
- Don’t immediately change from wearing mostly heels to wearing flats! If you’re accustomed to high heels and an unnaturally elevated arch, switching to flats cold turkey can be just as damaging as wearing heels in the first place. Wearing very high heels can cause the Achilles tendon to atrophy, meaning that when it’s stretched and worked harder in much lower flats, the chances of a break or tear are much greater. Lower your heel height gradually.
- Don’t be afraid to wear a little heel. Supportive shoes with a very slight heel can actually better for your feet than unsupported flats like ballet slippers, which can lead to flat feet. Heels should be 1-2 inches at the most.
- Fit is crucial. Many women make the mistake of buying heels that are too small for them. When wearing heels, it’s more important than ever to get the exact right fit.
- Keep in mind that slope is more important than height when looking at comfort and negative impact. Look for a thicker heel to distribute weight more evenly, and look for heels that are sloped gradually.
- Stretch your heels (the ones on the bottom of your foot!), plantar fascia, and calves before and after wearing heels to keep key muscles and ligaments strong and in good condition. (Try these easy stretches!)
- If you must wear high heels, try to wear them only to sitting events. And bring more supportive shoes to change into after the event–since the walk to and from the car is usually a significant part of the walking you’ll be doing!
If you wear high heels a lot–or are noticing pain in your feet or heels, it’s time to make some positive changes in your footwear to avoid further damage or injury. It’s also a great idea to incorporate slip-in orthotics to your footwear to cushion, support, and heal the damage caused by high heels. Wearing high heels might look fabulous, but it has nothing on the look–and feel–of healthy feet!
Benefits of Joining an Online Support Group for Plantar Fasciitis
 Suffering from chronic pain can feel very lonely at times. It can be extremely difficult for friends and family to understand, validate your feelings, and offer useful advice, despite their best efforts. This loneliness can be compounded by the pain itself. Some types of physical activity might be off limit at times, or you may need to simply rest your feet while other activities are happening.
Suffering from chronic pain can feel very lonely at times. It can be extremely difficult for friends and family to understand, validate your feelings, and offer useful advice, despite their best efforts. This loneliness can be compounded by the pain itself. Some types of physical activity might be off limit at times, or you may need to simply rest your feet while other activities are happening.
How can you meet your needs for support, advice, and validation? Online support groups are a great way to connect and bond with others who are in the same situation you are.
Benefits of Joining a Plantar Fasciitis Support Group
While plantar fasciitis is a relatively common condition, you might not know someone in your circle of friends or family who has been in your shoes, so to speak, in dealing with heel and foot pain. Finding support through an online community can be a huge help in the following ways:
Support: There’s a special kind of bond and support that is formed when we meet someone who has traveled a similar road or experienced a similar situation. And when it comes to chronic pain, that dynamic is no different. While friends and family may be very supportive and loving, you’ll gain a different type of support from others who suffer from chronic pain first-hand and speak your same language in a sense.

While friends and family can cheer you on from the stands, it can make a big difference to have the support of others who are in the arena with you, fighting the same battles you are.
Advice: In the same vein, those who don’t suffer from chronic pain may have a wealth of advice to offer, but suggestions and counsel from others who have tried the remedies or the therapy first-hand is invaluable. In a thriving online community, you’ll essentially be consulting a panel of experts for your questions and concerns. They might not be medical experts, but they’ve been walking the same path you have, and their input and advice can be incredibly helpful!
New Ideas: There’s nothing worse than feeling like you’re at the end of your rope or have tried everything when it comes to managing chronic pain. One of the greatest benefits of an online community is the constant influx of new ideas to try to better manage your pain and heal.
Can Online Support Groups Help with Chronic Pain and Depression?

The sense of community and support of an online support group can make a significant difference in your holistic health. Chronic pain and depression go hand in hand, and the physical symptoms you experience naturally take a toll on your mental well-being. However the good news is that the reverse is true as well. By taking steps to improve your mental health, your experience with chronic pain can change and improve as well. By becoming part of a community of others who are fighting similar battles and seeking help, you’ll find yourself not only gaining help and support yourself, but offering it to others, which can be an empowering and gratifying experience. You’ll also open a new door of possibilities and friendships.
Where Can I Find a Plantar Fasciitis Support Group?
Heel That Pain moderates an online Plantar Fasciitis Support group. Join us on Facebook, and find new ideas, new friendships, and support from others who understand what it’s like to deal with chronic pain.
Finding support online and offline can be a critical part of your healing process. Feeling understood, looking at your condition in new ways, and helping others along the way are some of the biggest benefits. Take the step to become part of the Plantar Fasciitis group today.