Everything You Need to Know About Plantar Fascial Thickening
 You may have heard that the thickness of your plantar fascia ligament is related to whether or not you have a condition called Plantar Fasciitis.
You may have heard that the thickness of your plantar fascia ligament is related to whether or not you have a condition called Plantar Fasciitis.
But what exactly does that mean? How thick is the average plantar fascia ligament? Why does the ligament get thicker in response to Plantar Fasciitis? How will you know if your plantar fascia is thicker than normal? And what can you do about all of it?
This blog post will cover everything you need to know about plantar fascial thickening.
Normal Plantar Fascia Vs. Thick Plantar Fascia
Just how thick is too thick? Several studies have shown that a healthy plantar fascia ligament runs between 2-4 mm thick in about 90% of people. Women usually have a thinner plantar fascia ligament than men (which may be another reason that women are more likely than men to get plantar fasciitis in the first place!)
Some outliers who don’t suffer from plantar fasciitis may have a plantar fascia ligament as thick as 5 mm. However, numerous studies have shown that for the most part, when the arch of the foot is thicker than 4 mm, there’s a very strong correlation with Plantar Fasciitis.
A study by Dr. Karabay MD, Dr. Toros MD, and Dr. Hurel MD, showed that individuals with heel pain had a plantar fascia thickness measuring an average of 4.79 mm.
Don’t worry: A thick arch doesn’t cause Plantar Fasciitis. It’s just a strong indicator that Plantar Fasciitis is present!
What Is Plantar Fascial Thickening, and Why Does It Happen?
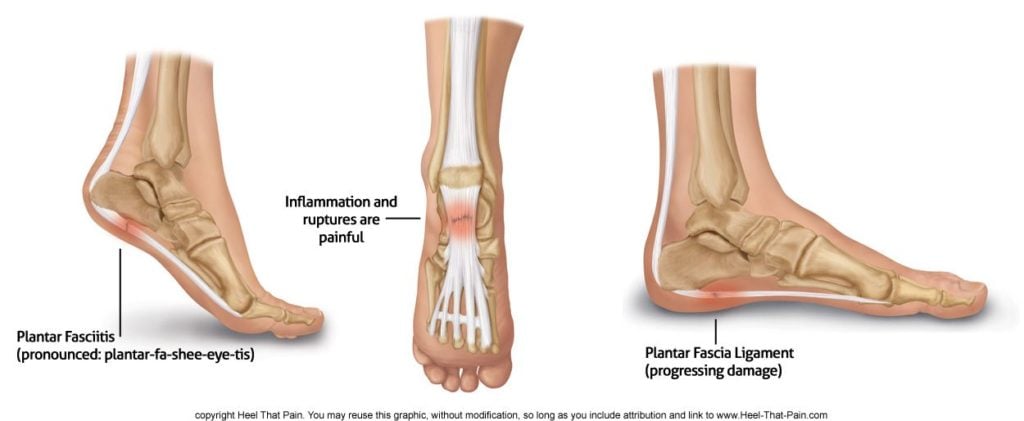
A thicker plantar fascia ligament often goes hand in hand (well, foot in foot) with a diagnosis of Plantar Fasciitis for a couple of reasons:
- Wear and Tear: Plantar fasciitis is caused by wear and tear, trauma, tiny injuries, or overuse of the plantar fascia ligament. A healthy arch distributes weight and absorbs impact sort of like a spring. But with enough trauma, overuse, and injury that spring will collapse–and the feet will flatten. Research from Chang Gung Memorial Hospital has shown that flat feet are related to plantar fascial thickening. Some experts speculate that this tissue thickening happens for the same reason a callus or bunion develops–too much use, pressure, or damage.
- Scar Tissue: Scar tissue can be another reason why the plantar fascia ligament might be thicker than usual. Over time, as the body attempts to support and heal the damaged fascia, tiny lesions and scar tissue can build up, adding extra bulk.
- Swelling: Inflammation and swelling in the area may lead to a thicker plantar fascia ligament.
Identifying a Thickened Plantar Fascia
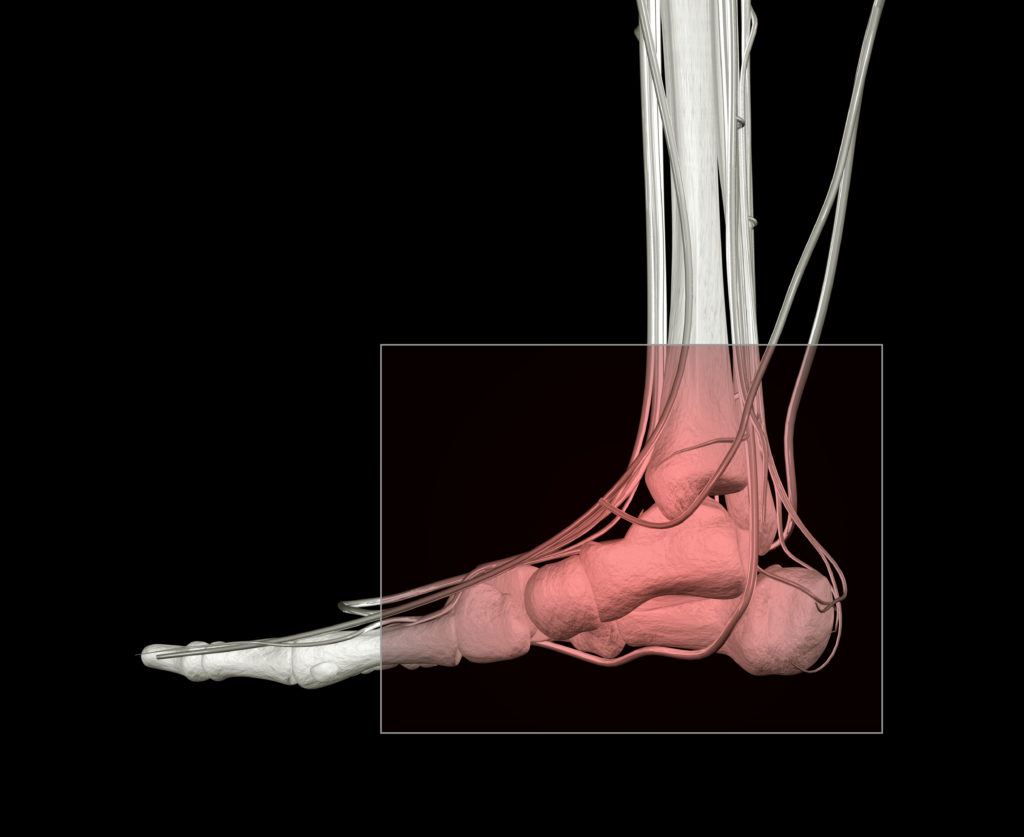
MRI or ultrasound imaging are two of the most common tools doctors will use to see if the plantar fascia is thickening. These tools show a clear picture of soft tissues in the foot including muscles, ligaments, and tendons.
MRI and ultrasound can also help rule out stress fractures, as well as pinpoint erosion of the fatty heel pad (another telltale sign of Plantar Fasciitis) and heel spurs. Identifying a thickened plantar fascia can help your doctor confirm a diagnosis of plantar fasciitis, since this is one of the most reliable indicators of the condition.
How Can You Prevent Plantar Fascial Thickening?
The best way to prevent plantar fascial thickening is to keep the arch of your foot healthy, supported, and rested.
- Try to avoid long periods of standing when possible
- If your feet or heels hurt or look red and swollen, ice them to bring down the pain and inflammation
- Maintain a healthy body weight when possible, to avoid putting excess strain on your arch
- Wear high-quality orthotic insoles to cushion and support your arches when standing or walking
- Stretch your feet, ankles, and legs to improve strength and flexibility in your arch and supporting muscles and ligaments
Most people don’t have any idea they have a thickened plantar fascia ligament–until heel pain strikes. Thankfully, with easy at-home preventative treatments like these, you can maintain your arch health–and avoid plantar fascial thickening!
Radiation Therapy for Plantar Fasciitis
 Radiation therapy, also known as radiotherapy, is a medical treatment that uses a targeted dose of radiation (a type of energy) to break down certain types of tissue in the human body.
Radiation therapy, also known as radiotherapy, is a medical treatment that uses a targeted dose of radiation (a type of energy) to break down certain types of tissue in the human body.
Higher doses of radiation are commonly used to shrink cancerous tumors. Lower doses of radiation, on the other hand, can be used to break up scarring and damaged tissue in the ligaments of the heel and arch.
An important study by Dr. Robert Michael Hermann, MD, found that radiation therapy is an effective non-invasive treatment method for a high percentage of plantar fasciitis patients. Here’s what you need to know before you decide to give radiotherapy a try!
What Is Radiation Therapy (Radiotherapy)?
Radiation therapy uses the same kind of energy that’s used in X-rays to damage or destroy certain kinds of tissue.
While radiation therapy might sound a little intimidating–since it’s the same type of therapy used to treat breast and prostate cancer patients–you should know that the radiation therapy for Plantar Fasciitis is delivered in a much lower dose.
Radiation is measured in units of (Gy). Cancerous tumors are usually targeted with a dose of approximately 60 or 70 Gy per treatment (high enough to break down the DNA and molecules of a cancerous tumor). Plantar Fasciitis, on the other hand, is usually targeted with a dose of only 3 Gy–about 20 times less.
What to Expect From Radiotherapy for Plantar Fasciitis

One of the most common concerns about radiotherapy for Plantar Fasciitis is the potential side effects. Many people are aware of the unpleasant side effects that sometimes happen from higher-dose, tumor-targeting radiation, which can include hair loss, fatigue, and skin irritation.
However, it’s important to understand that the tiny dose of radiation delivered during radiotherapy for Plantar Fasciitis won’t cause these side effects. Radiotherapy itself is very quick and completely painless, and may take as little as five minutes.
In the days following radiotherapy for Plantar Fasciitis, you may notice a small amount of swelling or redness, which will pass quickly. However, you will be able to walk as you normally do. (Remember to wear orthotics to support your healing arch and avoid reinjury!)
In general, radiotherapy treatments for Plantar Fasciitis are administered once or twice a week, for a course of six to eight weeks. The cost of radiation therapy will vary depending on your insurance coverage, but many insurance companies cover the procedure, and you may only be responsible for a copay.
Is Radiation Therapy Effective for Plantar Fasciitis?
The reason radiotherapy is effective at destroying cancerous tumors is that the targeted radiation completely completely destroys cancer cells. This high dose of radiation will, of course, also damage normal cells. However, these normal cells have the ability to repair themselves–while the cancer cells do not.
When it comes to Plantar Fasciitis, low doses of radiation break down painful scar tissue in the heel and arch. The small dose of radiation can also trigger a healing response, as the cells that have just sustained some damage repair themselves.
In a recent study by Dr. Hermann MD, 200 patients were treated with radiation therapy for Plantar Fasciitis. Three months after the course of radiation therapy, almost 70% were pain free or had very little pain. At 54 months, a little over 60% were still pain-free or almost pain free.
Are You a Good Candidate for Radiation Therapy?
While most cases (over 90%) of Plantar Fasciitis respond well to conservative treatments such as orthotics, physical therapy, icing, and stretching, other cases are more stubborn.
For chronic, complex, or debilitating cases of Plantar Fasciitis, surgery may seem like the only option left. But if you’ve tried conservative options without success, noninvasive radiation therapy can be a great option before you undergo the expense, pain, and recovery of Plantar Fasciitis surgery.
If you’re considering radiation therapy for Plantar Fasciitis, talk to your doctor about your questions and concerns–especially if you’re looking at having surgery. While everyone’s health and circumstances are different, radiation therapy shows a great deal of promise as a less expensive, less invasive alternative to surgery.
Diagnostic Imaging for Heel Pain: X-Ray, MRI, Ultrasound, CT-Scan
 Diagnostic imaging can be an invaluable tool for treating and diagnosing heel pain, allowing doctors and healthcare providers a literal look beneath the surface.
Diagnostic imaging can be an invaluable tool for treating and diagnosing heel pain, allowing doctors and healthcare providers a literal look beneath the surface.
What are the different types of imaging commonly used for Plantar Fasciitis and heel pain? When is diagnostic imaging needed? And what can you expect from imaging in terms of cost and experience?
This blog post will answer common questions and help you make a more informed decision about diagnostic imaging with your healthcare provider.
When Is Diagnostic Imaging Needed?
If you’re dealing with Plantar Fasciitis or heel pain for the first time, your doctor isn’t likely to recommend an X-ray or MRI. A review of your health history, lifestyle, and a physical exam can usually provide your doctor with everything he or she needs to know for a diagnosis.
In general, diagnostic imaging is used for Plantar Fasciitis and heel pain in two common situations:
Stubborn or Chronic Plantar Fasciitis
While an amazing 90% of Plantar Fasciitis cases respond well to conservative treatment methods, the remaining 10% can be very stubborn or chronic. In this case, your doctor may use diagnostic imaging to take a closer look at the mechanics of your foot, to determine why your heel pain is resistant to treatment, and how to move forward.
Ruling Out Other Conditions
Several foot conditions can masquerade as Plantar Fasciitis. Depending on your symptoms and medical exam, your doctor may decide that diagnostic imaging is needed to rule out tendonitis, bursitis, a stress fracture, a plantar fascia tear or rupture, nerve entrapment, tarsal tunnel syndrome, and so forth.
Plantar Fasciitis that has a very sudden or dramatic onset, is accompanied by pain that doesn’t respond to conservative treatments, or gets worse with conservative treatments is likely to result in diagnostic imaging.
Types of Imaging Used for Heel Pain
If you have recalcitrant Plantar Fasciitis (heel pain that just won’t go away), or your doctor suspects that your heel pain may be something other than Plantar Fasciitis, he or she may recommend one or more of the following imaging options.
If your doctor recommends imaging that you feel is unnecessary, or prior to trying conservative treatment methods, don’t be afraid to get a second opinion or ask more questions! Knowing what types of imaging are available–and what each type of imaging can accomplish–will help you be an effective advocate for your health.
Ultrasound (Sonography)
A diagnostic ultrasound, also called a sonogram, is a quick and easy imaging method used to take a look at soft tissues in the foot (not to be confused with Ultrasound Therapy for treating Plantar Fasciitis). This imaging tool can rule out soft-tissue conditions like tendonitis, tarsal tunnel, nerve compression, and plantar fibromatosis.
Ultrasound can also show whether or not the fatty heel pad looks normal, and whether the plantar fascia is thicker than normal (thicker than 4 mm), flattening, deteriorating, or compromised by micro-injuries and small tears.
X-Ray (Radiograph)
X-rays aren’t typically used to diagnose Plantar Fasciitis, since they don’t offer a good look at soft tissues. They can, however, be very valuable in ruling out or confirming a stress fracture.
X-rays can also be used to look for heel spurs or bone spurs on the foot that are digging into the fatty pad of the heel and causing pain, evidence of arthritis, or problems with alignment in the foot.
MRI (Magnetic Resonance Imaging)
An MRI uses a magnetic field combined with radio waves to provide detailed cross-section images of bones, tendons, and soft tissues. Unlike an X-ray or ultrasound, MRIs can take up to an hour, and require the patient to remain very still.
MRIs can pinpoint plantar tears or ruptures, tendon injuries, lesions, cysts, and sometimes fractures or heel spurs, without the radiation and expense of a CT-scan. MRIs are also sometimes used to confirm Haglund’s Deformity and Achilles tendonitis.
CAT-Scan (CT Scan)
A CT scan or CAT scan is a special type of X-ray with the ability to capture a detailed cross-section of your foot, including soft tissue and bones. However, CT scans aren’t typically used to diagnose or treat Plantar Fasciitis unless your doctor is concerned about tumors on the heel or calcaneus.
CT scans are more expensive, expose patients to a small amount of radiation, and generally do not provide more information than an MRI or X-ray for Plantar Fasciitis or other conditions that cause heel pain.
What to Expect from Imaging for Heel Pain

Knowing what you can expect from imaging will help you feel prepared, and may also help you make a decision about whether a particular kind of imaging is right for you.
What Does Imaging Feel Like?
All of the types of imaging covered in this blog post are painless. However, it’s important to understand that some types of imaging may still cause stress or discomfort because of the equipment, positioning, and time required for successful images.
Ultrasound and X-ray are the quickest and easiest forms of imaging. Both of these tools take just a few minutes.
A CT-scan usually takes 5-20 minutes, and requires patients to place the foot and leg into a narrow tube. Since CT-scans emit a small dose of radiation, they usually aren’t recommended for children, or pregnant women.
MRI scans take the longest, which can sometimes cause discomfort from laying on the hard table. The process can take between 30-60 minutes, and it’s important to stay very still. The machine makes loud knocking sounds while it works, which can be unsettling for some patients, and it may not be recommended for patients with tattoos, pacemakers, or metal screws or plates in the foot and leg.
Cost of Imaging
The cost of imaging for Plantar Fasciitis can vary quite a bit, depending on your insurance coverage and whether you get the imaging done in a doctor’s office or a hospital. Don’t be afraid to call ahead and ask about costs and discounts for same-day payment. If you can, verify whether your provider and the procedure is covered by your insurance before you havre the imaging done.
In general, imaging done in a doctor’s office will be less expensive than imaging done at a hospital. Ultrasound and X-rays are usually the least expensive imaging options, followed by MRI and CT-scans.
Remember, if this is your first experience with heel pain or Plantar Fasciitis or heel pain, imaging usually won’t be needed.
Resting your feet, icing, stretching, and supporting your arch with orthotic insoles helps most people heal within a few weeks to a few months. However, if you or your doctor don’t see results with conservative treatment, or you suspect your heel pain may be something other than Plantar Fasciitis, imaging can be an invaluable tool in making a correct diagnosis.
Laser Therapy for Plantar Fasciitis
 A laser is an intense, focused beam of light that can become a powerful medical instrument in the hands of a skilled doctor. Cosmetic surgeons, oncologists, dermatologists, and opthamologists are just a few of the medical providers who use lasers to treat a wide variety of conditions.
A laser is an intense, focused beam of light that can become a powerful medical instrument in the hands of a skilled doctor. Cosmetic surgeons, oncologists, dermatologists, and opthamologists are just a few of the medical providers who use lasers to treat a wide variety of conditions.
In recent years, podiatrists have begun using laser therapy to treat Plantar Fasciitis and heel pain. The precision of modern laser therapy offers a non-invasive alternative to surgery that may relieve pain and promote healing of Plantar Fasciitis
If you or a loved one suffer from Plantar Fasciitis, the following information can help you decide whether laser therapy is right for you:
What Is Laser Therapy for Plantar Fasciitis?
There are two main kinds of laser therapy that can be used to treat Plantar Fasciitis: low-level laser therapy (also called LLLT, or “cold laser therapy), and high-level laser therapy (also called “hot laser therapy). It’s important to understand that even among “cold lasers,” different brands have different beam types, pulse speeds and purported effectiveness.
Both types of laser therapy involve moving a highly focused beam of light over the plantar fascia in an effort to stimulate cellular metabolism, protein synthesis, wound healing, and immune response. The depth of the laser’s reach and its effectiveness can vary depending on the type and brand of laser used.
Low-Level Laser Therapy (AKA, Cold-Laser Therapy)
This treatment for Plantar Fasciitis has been approved by the FDA and is covered by most insurance companies. Low-level laser therapy is also called “cold-laser therapy,” since the pulse of the laser (a Class III laser) is so low that almost no heat is generated. Most people report feeling no pain during the procedure.
According to some doctors, patients may feel immediate relief from their heel pain, and some studies show that low-level laser therapy can be effective when combined with conservative treatments like stretching and orthotics. Other clinical trials show no difference in healing when compared with placebo. However, anecdotal evidence for the effectiveness of low-level laser therapy is strong, and many people report pain relief and long-term positive outcomes.
High-Level Laser Therapy (AKA, Hot Laser Therapy)
As the field of laser therapy has grown, some doctors now prefer to use Class IV lasers instead of Class III lasers to perform laser therapy for Plantar Fasciitis. This stronger beam can penetrate deeper into the tissue and is often called “hot laser therapy,” since the stronger laser produces more heat.
This procedure can be more painful, and some doctors believe that it unnecessarily damages healthy tissue. However, other doctors insist that the more powerful laser is necessary to penetrate the fascia deeply enough to treat the injury effectively. One industry-sponsored study showed that 80 percent of patients treated with a Class IV laser improved their Plantar Fasciitis.
Is Laser Treatment Effective for Plantar Fasciitis?

There’s plenty of differing opinions about laser therapy in the field of podiatry. Some doctors advocate for laser therapy (either hot or cold), while others insist that the treatment is a waste of time. Laser therapy appears to be extremely effective for some individuals, while ineffective for others.
If you’re considering laser therapy for Plantar Fasciitis, it’s important to talk to your doctor and manage your expectations. However, since laser therapy is inexpensive and relatively painless, many people consider it a worthwhile experiment before surgery, or a useful supplemental treatment in combination with tried-and-true conservative treatment methods for Plantar Fasciitis.
Pros and Cons of Laser Therapy
Both hot and cold laser therapies are safe, non-invasive, and relatively painless. The main drawback for both types of laser therapy is the mixed reports of laser therapy’s effectiveness; however, improved modern lasers may be more more effective in targeting and treating the damaged fascia, and new studies show more promise for laser therapy.
Pro: Safe, with Minimal Side Effects
Laser therapy comes with almost zero potential for negative side effects. You may experience mild redness, inflammation or swelling immediately after the procedure, especially for hot laser therapy; however, icing and NSAIDs can be used as needed.
Pro: Non-Invasive, Minimal Pain, and Fast Treatment
Cold laser therapy is virtually painless. Hot laser therapy may be more painful, but is usually reported as being tolerable without anesthesia. Some people describe the sensation as a hot rubber band being snapped on the bottom of their foot. Both types of laser therapy require only a few minutes per treatment.
Pro: Inexpensive
Since most insurance companies cover laser therapy, the cost may be as little as a copay. Most doctors recommend a series of 6-12 treatments over the course of several weeks. Compared to surgery, which may cost thousands of dollars, laser therapy is significantly less expensive.
Con: Mixed Evidence of Effectiveness
While earlier studies and clinical trials found little evidence of laser therapy’s effectiveness, some doctors point to poorly designed clinical trials and older laser models. Modern lasers are more powerful, more precise and appear to show potential for healing and pain relief.
Make sure to ask what brand of laser your doctor uses, and do you research to find out if others have had positive experiences with that particular brand. You’ll also want to find out whether your doctor is using a Class III (cold laser therapy) or Class IV laser (hot laser therapy).
6 Mistakes To Avoid When You Have Plantar Fasciitis
 With any injury, it’s critical to promote healing while avoiding re-injury or relapse. That’s why knowing what not to do when you have Plantar Fasciitis is just as important as knowing your best treatment options.
With any injury, it’s critical to promote healing while avoiding re-injury or relapse. That’s why knowing what not to do when you have Plantar Fasciitis is just as important as knowing your best treatment options.
If you have Plantar Fasciitis (or you think you might have Plantar Fasciitis) don’t make these six common mistakes. They could cost you a longer recovery time, expense, pain, and additional complications!
1. Jumping Straight to Expensive Treatments
If your doctor recommends surgery the first time you make an appointment to talk about heel pain, proceed with caution (more on that coming up). An incredible 90% of Plantar Fasciitis cases can be successfully resolved without surgeries, many using inexpensive, conservative treatments in the comfort of your own home.
While heel pain can feel so bad, and so serious that surgery seems like the only reasonable option to fix it, take comfort in knowing that most people are able to heal without the trauma and expense of surgery or medical interventions. Tried-and-true conservative treatments like icing, stretching, sock splints, and wearing orthotics made just for Plantar Fasciitis are the very best frontline defense.
2. Not Seeking a Second Opinion
If you don’t feel heard or comfortable with your podiatrist or doctor, get a second opinion. While there are some generally agreed-upon principles of treating plantar fasciitis, each person and each situation is unique.
If your own research or situation don’t seem to be jiving with your current doctor, it’s okay to respectfully find other care. Ask for reviews in local Plantar Fasciitis support groups, or do some more research online to find a doctor who’s a good fit. You are the best advocate for your own health, and you should always feel comfortable asking questions and questioning proposed treatment plans.
3. Waiting to Treat Your Plantar Fasciitis
Like other injuries, it’s important to take corrective action quickly if you suspect that the arch of your foot may be damaged. Continuing to walk, run, or jump with a damaged fascia can make micro-injuries worse, allow the arch to flatten further, and increase the time required for healing.
Treating heel pain right away using conservative treatment methods like orthotics, icing, and stretching is one of the best ways to avoid costly and more invasive medical interventions down the line. When in doubt, talk to your doctor, rest from any physical activities that are causing pain, and begin conservative treatments.
4. Spending Lots of Time (and Money) on Miracle Cures
In the age of the Internet, all it takes is a few clicks to find treatments “guaranteed” to cure Plantar Fasciitis–for a price, of course. However, research often reveals that these miracle cures are heavy on marketing and a little more ambiguous on results.
If a new treatment is inexpensive and doesn’t have harmful side effects, it probably won’t hurt to try. However, be skeptical of expensive and very new “miracle” treatments for heel pain that are getting a lot of buzz online. Remember, most cases of Plantar Fasciitis can be successfully treated using very inexpensive at-home remedies. Before trying other treatments, do your research to find real user reviews, any research that backs the new treatment, and the track record of the company that is promoting the new treatment.
5. Using Ice or NSAIDS the Wrong Way
While icing and non-steroidal anti-inflammatory drugs like ibuprofen can be extremely helpful in temporarily relieving pain, it’s possible to use them the wrong way.
Apply ice indirectly to the skin, to avoid frostbite (using a plastic bag wrapped in a paper towel, or handy ice slippers to avoid the mess). And keep the ice applied for between 10 and 20 minutes, to maximize the benefits of numbness and reduced inflammation. However, keeping the ice on your skin longer than 20 minutes can actually cause tissue damage and problems with circulation.
When it comes to NSAIDs, don’t make the mistake of using them to temporarily relieve your pain–so you can engage in activities that might make your Plantar Fasciitis worse, like jogging or a rowdy game of basketball. Pain is your signal that something is wrong. Respect the pain, and treat it as needed with NSAIDS–but not as a way to push through!
6. Inconsistent Conservative Treatments
Tried-and-true home remedies for Plantar Fasciitis are only as good as the consistency with which they are applied. Stretching once a week for a couple of minutes won’t build the strength and flexibility your arch, calves, ankles, and legs need to absorb and distribute impact properly. And wearing orthotic insoles once in a while–or keeping your favorite pair of high heels in constant rotation–may result in chronic Plantar Fasciitis.
Wear orthotics or wrap your heels whenever possible, and stretch once or twice each day for 10-20 minutes. As needed, use ice and NSAIDs for pain, and give your feet plenty of rest.
It’s important to understand that you probably won’t see results immediately from conservative treatments. While orthotic insoles offer immediate pain relief for many people, healing the underlying condition of Plantar Fasciitis takes time to resolve–just as it took time to develop.
By avoiding these six mistakes and staying consistent with your at-home treatments, it’s not only possible but extremely likely that you’ll find healing and relief from your heel pain.