Plantar Fasciitis vs. Stress Fractures
 You had a hard workout yesterday and wake up to find that your heel pain is absolutely unbearable.
You had a hard workout yesterday and wake up to find that your heel pain is absolutely unbearable.
Making a quick assessment of your situation is important so that you can get the treatment you need, avoiding additional injury, and preventing long-term damage.
But both Plantar Fasciitis and stress fractures can involve intense heel pain that makes weight-bearing activities difficult.
So is it Plantar Fasciitis, or is it a stress fracture?
Each of these two conditions has unique hallmarks that will help you and your doctor make a quick and accurate diagnosis:

Do You Have Plantar Fasciitis?
The thick, flexible tissue connecting your heel to the ball of your foot (AKA the arch of your foot) bears the brunt of the impact and distributes the weight of your body as you walk, run, or jump. When the plantar fascia becomes damaged through overuse or injury, this band of tissue can sustain small tears or become inflamed. When that happens, you have a condition called Plantar Fasciitis.
Causes of Plantar Fasciitis
Plantar fasciitis is caused by overuse or injury to the arches. The subsequent inflammation and damage results in heel pain that can be excruciating, especially the first thing in the morning. Plantar fasciitis can be caused or exacerbated by any of the following:
- Intense exercise sessions, especially if the muscles are ligaments aren’t properly warmed up
- Weight gain that results in additional strain and impact to the arches
- Walking, standing, or running without supportive foot and arch support
- Flat or high arches that don’t allow for proper weight distribution in the feet
Symptoms and Telltale Signs of Plantar Fasciitis

The biggest telltale sign of Plantar Fasciitis (and one of the best ways to distinguish it from a stress fracture) is that the pain is worse with those first few steps in the morning, that improves slightly with use and movement as the fascia stretches and warms up.
Other classic symptoms of Plantar Fasciitis include the following:
- Achy, stiff heels and arches
- Redness, swelling, and inflammation in the heel and along the arch
- Pain that is worse in the morning or after inactivity
- Pain that improves with rest, stretching exercises, and icing
- Persistent dull pain, or sharp, needle-like pain that may cause you to limp
Diagnosing Plantar Fasciitis
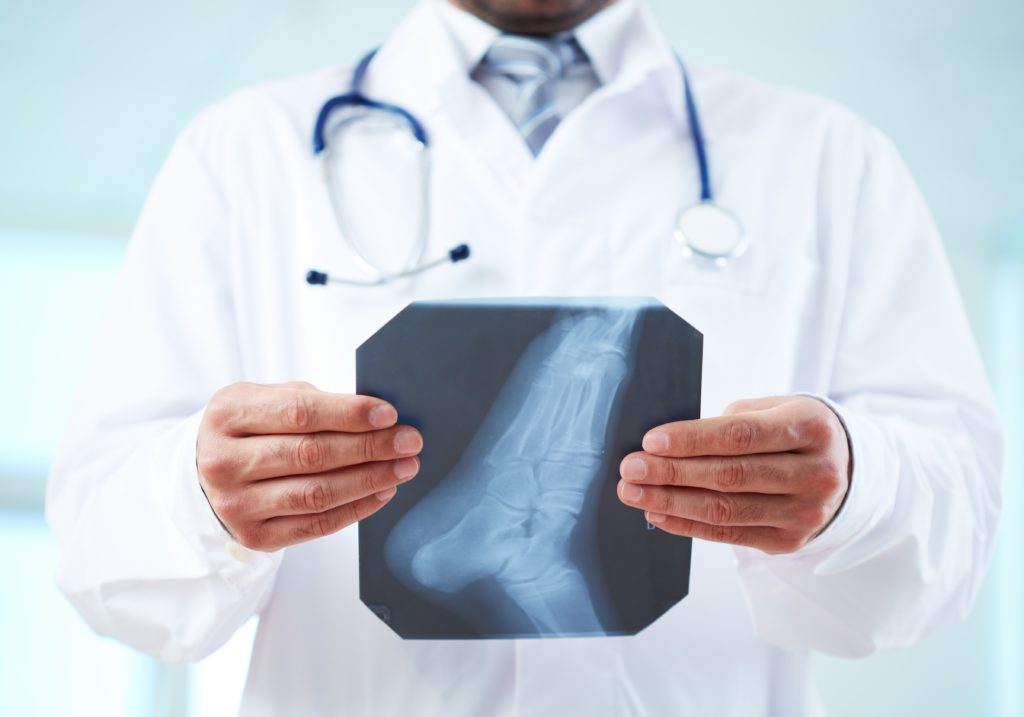
Your doctor will diagnose Plantar Fasciitis based on your lifestyle, medical history, and an examination of your heel and arch. If a stress fracture is suspected or needs to be ruled out, your doctor will also probably take x-rays. While x-rays can’t always confirm Plantar Fasciitis, your doctor will look for thickening and inflammation of the plantar fascia, as well as the presence of heel spurs (rigid calcium deposits on the heel bone in response to trauma and inflammation). However, heel spurs are not found in all cases of plantar fasciitis.
Treatment for Plantar Fasciitis
More than 90% of plantar fasciitis cases can be successfully resolved with conservative treatment methods to reduce inflammation better support your arches:
- Regular stretching
- Icing the heel and plantar fascia
- Shoes that fit properly and support your heel and fascia
- Regular use of orthotics like Heel Seats
- Changes to your diet (to avoid inflammatory foods and maintain a healthy weight)
- Anti-inflammatory medication to manage pain, including ibuprofen
Unlike Plantar Fasciitis, the pain from a stress fracture usually gets worse with physical activity. While a stress fracture can result from the same causes and activities as plantar fasciitis, a fracture must be treated differently to avoid further damage and pain.
Do You Have a Stress Fracture?

Like Plantar Fasciitis, stress fractures are often caused by overly intense exercise, overuse, and high impact. However, while plantar fasciitis is an injury to a ligament in the arch of the foot, a stress fracture is a small crack or fissure in one of the bones in the heel or foot.
Causes of Stress Fractures
Stress fractures can be caused by overuse, injury, or the overall condition of your bones. If you have osteoporosis, are taking medication that makes your bones more fragile, or are deficient in Vitamin D, it’s possible to sustain a stress fracture even during normal daily activities. Stress fractures are often caused by the following factors:
- Increasing the intensity of a workout or sports activity without warming up gradually or building endurance
- Not allowing for proper rest between workouts
- Running, walking, or exercising on hard, uneven surfaces
- Wearing shoes that don’t fit properly, or don’t provide proper cushioning and support
- Osteoporosis or medications that weaken the bones
- Diets that are deficient in Vitamin D and calcium
- Trauma
Symptoms and Telltale Signs of Stress Fractures
While the pain from plantar fasciitis can have a rapid onset in some cases, the pain typically increases gradually. With a stress fracture, you’ll likely notice a more sudden onset of intense pain. Stress fractures can be the result of a fall or sudden impact, or they may be the result of vigorous exercise regimens that don’t allow the bones in the heel or foot to heal from micro-injuries over time. You should also look for these telltale symptoms:
- Pain that gets worse the longer you’re on your feet
- Intense pain that is localized to one spot on the heel or foot, and is tender to the touch
- Redness and swelling at the fracture site
- Pain that gets worse with stretching
Diagnosing a Stress Fracture

If you suspect you have a stress fracture in your heel or foot, it’s important to get medical attention right away to avoid further damage or a full break in the bone. Your doctor will examine your foot and will likely take x-rays to confirm the fracture. Since stress fractures are very tiny, it’s sometimes difficult to see them on an x-ray. If your symptoms indicate a stress fracture, your doctor may decide to treat you for this condition regardless of whether the fracture shows up on an x-ray.
Treatment for Stress Fractures
While you wait for your doctor’s appointment, do everything possible to avoid further damage or a complete break in the bone. Rest your foot, ice the area for 10-15 minutes in intervals throughout the day, wrap the foot with KT tape or an Ace Bandage for stability, and elevate the foot to reduce swelling. Try to avoid putting weight on the area as much as possible.
Your doctor’s recommended course of treatment will depend on the severity of your fracture and your unique circumstances. He or she may recommend a cast, crutches, or a strict regimen of rest while the fracture heals. This will take between 6 to 8 weeks at a minimum. It’s important to follow your doctor’s recommendations, even if you start feeling better, to allow your foot to completely heal. You can take anti-inflammatory painkillers like ibuprofen during the healing process as needed. As you heal, and once you are back on your feet, it’s also more important than ever to wear protective, supportive footwear to avoid re-injury or further breakage. In fact, it’s not uncommon for plantar fasciitis to develop soon after a stress fracture heals.
Whether you’re dealing with a stress fracture or Plantar Fasciitis, getting treatment as soon as possible will help you relieve the pain you’re experiencing and avoid more damage to your feet and heels.
When is Heel Pain an Emergency?
 Heel pain can be extreme in many situations–there’s no question about that.
Heel pain can be extreme in many situations–there’s no question about that.
But it’s not always simple or easy to decide whether your level of pain requires at-home treatment, a trip to the doctor, a visit to urgent care, or a trip to the emergency room.
When severe pain strikes, how can you decide whether your situation warrants a trip to the emergency room versus urgent care or your family doctor?
The following guidelines can be helpful in deciding your best course of action for quick relief and long-term healing:
When to Visit the Doctor for Heel Pain
Typically, your primary care physician or podiatrist is your best bet for treating severe heel pain that doesn’t require an emergency room visit (more about that below!). If you’re experiencing any of the following symptoms, it’s important to schedule a visit with your doctor right away:
- Heel pain that doesn’t respond to conservative at-home treatments for plantar fasciitis like icing, orthotic inserts, rest, and stretching
- Heel pain and foot pain that suddenly becomes worse
- Numbness in your feet or heels
- Pain even while you aren’t putting weight on your feet and heels
Depending on your diagnosis and unique situation, your doctor may still decide to refer you to a hospital or recommend surgery. But if your situation is ongoing and can wait just a few hours or even a day or two, it’s a good idea to start with the professional who knows your health history best. And don’t be deterred by previous wait times: Even if you’ve previously had to wait a couple of weeks for an appointment with your doctor or podiatrist, call anyway and explain what’s going on. Most doctors will make room in their schedule based on the severity of your symptoms, especially if you are a current patient.
When in doubt as to whether your situation needs to be addressed immediately at an urgent care or in the emergency room, call a 24/7 nurse hotline (most insurance networks and hospital networks provide this free service).
Cost/Benefit: A standard doctor’s office visit is likely to be your least expensive option for dealing with severe heel pain with a standard copay or out-of-pocket payment; however, it’s not usually the most immediate solution.
When to Visit Urgent Care for Heel Pain
Urgent care clinics exist primarily to fill the gap when your doctor’s office is closed for the day, and you need to be seen immediately. If your heel pain increases in severity or you are concerned about the onset of new symptoms alongside your heel pain, but aren’t certain you have an emergency on your hands, urgent care is a good choice.
At urgent care, you may be given pain medication or other treatments to manage your condition until you can be seen by your primary care provider. Urgent care providers are also trained to determine whether a situation is severe enough that you need medical treatment in a hospital setting immediately. If your situation does merit a true emergency, you’ll be referred to an emergency room immediately. However, if your situation doesn’t merit emergency treatment, you’ll have peace of mind knowing that your condition isn’t likely to deteriorate by waiting for your primary care physician’s office to open.
Urgent care facilities can often perform simple x-rays, but are not equipped to offer on-the-spot surgery.
If you’re experiencing any of the following symptoms, get to your doctor (if the office is open) or urgent care (if your doctor is not available) right away:
- An increase in heel pain severity accompanied, by a fever
- Severe inflammation in the heel and foot area with red streaks spreading away from the area
- Heel pain that suddenly gets much worse
Cost/Benefit: The cost of an urgent care clinic will typically be higher than your doctor’s office copay or out-of-pocket expense, but not by much. Expect to pay approximately twice what you might pay for a standard doctor’s visit for the benefit of after-hours service.
When to Visit the Emergency Room for Heel Pain

In general, the emergency room is the right choice if your situation feels like “every minute counts” in how quickly the symptoms have onset, how quickly your condition is deteriorating, or how likely failure to treat your symptoms might result in permanent damage or disability.
The emergency room is equipped to handle situations that must be resolved quickly and immediately, can’t wait for a primary care provider’s diagnosis, might require immediate surgery or medical intervention, or might result in dire consequences if left untreated.
It’s important to remember that ER doctors are experts in putting the brakes on an emergency, not providing specialized foot care. If your symptoms don’t require emergency treatment, it’s highly likely that you’ll be referred to a specialist who can help you treat your condition effectively. However, if you experience any of the following symptoms the ER may be the right choice:
- Lacerations of the heel or foot with heavy bleeding
- A suspected torn Achilles tendon, marked by a popping sound in the heel or foot, followed by severe pain and inability to bear weight
- Sudden inability to move or bear weight on the heel or foot, accompanied by fever, chills, and nausea
- A diagnosis of diabetes accompanied by a laceration or injury to the heel that is inflamed, warm to the touch, or worsening in severity
- Signs of a stress fracture (which may break completely if not addressed quickly) or broken bone in the heel or foot: inability to bear weight, swelling, and extreme pain
Cost/Benefit: The emergency room is almost certainly the most expensive option available, easily running into the thousand-dollar range for the visit alone. However, in a true emergency it’s an invaluable resource to avoid permanent damage or serious consequences for your health.
When in doubt, trust your instincts and err on the side of your health. If you’re feeling conflicted about what to do in your unique situation, don’t be afraid to call your doctor’s office, the urgent care facility, or the 24-7 nurse hotline before you make the trip. When you’re in pain, it can be especially difficult to make a decision that will impact not only your pain level but your finances.
Take a few minutes to rest, breathe deeply, and evaluate the situation. Then consider the information above, talk to a live medical professional, and seek the help you need. No matter what your level of pain, “grin and bear it” shouldn’t be among the options you consider. Pain is your body’s way of alerting you to a serious situation that needs to be addressed–and the more acute and sudden the onset of the pain, the more aggressively your body is trying to relay the message that serious damage may be occurring.
What to Expect: Physical Therapy for Plantar Fasciitis
 When it comes to health, nobody likes surprises.
When it comes to health, nobody likes surprises.
Knowing what to expect from a procedure or treatment plan not only helps you determine whether it’s actually the right course of action for your situation; it also helps you prepare yourself mentally, emotionally, and financially.
The term “physical therapy” can mean a LOT of different things, depending on the type of physical therapy, the condition being treated, and the therapist you choose.
Learning what to expect at a physical therapy session for plantar fasciitis, how to choose a physical therapist that’s right for your situation, the average cost of physical therapy, and the types of stretches and exercises you can expect will help you make informed decisions and set your mind at ease:
What Is Physical Therapy?
For the majority of people, physical therapy for plantar fasciitis becomes a consideration after foot surgery, or if more conservative treatment methods aren’t working.
Physical therapy is a combination of supervised manual therapy and a personalized treatment plan intended to restore mobility, reduce pain, and improve the health of the arch. Physical therapists typically have a degree in health sciences, nursing, sports medicine, or physical therapy. No matter which physical therapist you choose to help you recover from surgery or improve your difficult-to-treat plantar fasciitis, you can expect assistance in the following ways:
- One-on-one, supervised guidance as you work through a series of stretches and exercises to improve mobility, flexibility, and arch strength
- A resource for education about your unique situation
- Access to treatments like electrical stimulation and ultrasound, as they are needed
- Help create a plan for at-home physical therapy to supplement in-office physical therapy
Before you start physical therapy, you’ll want to make sure that you’ve dotted your i’s and crossed your t’s for insurance purposes. Some physical therapists require a referral from another physician, while others don’t. If you’re undergoing physical therapy after surgery for plantar fasciitis, you’ll want to be sure to arrange and confirm everything before your surgery to avoid expensive surprises post-op.
Choosing a Physical Therapist for Plantar Fasciitis

While every physical therapist’s goal is to help you recover and literally get back on your feet, there’s a wide variety of physicians and practice types to choose from.
Do some research online and stop by a few offices to get a flavor of the types of practices in your area. Some will be quite small and intimate, with only one or two physical therapists on staff. Others will employ many physical therapists and may be part of a large hospital network. While your choice of physician is the most important, you’ll also want to choose a location, organization, and environment you feel comfortable with.
When choosing your physical therapist, look for reviews online and ask for suggestions in local support groups for plantar fasciitis. When possible, find a physical therapist who specializes in rehabilitating the feet and arches. Don’t be afraid to ask about costs upfront, and to make sure that your insurance is covered, if you have it.
What to Expect at Physical Therapy for Plantar Fasciitis
The biggest question most people have about what to expect from physical therapy for plantar fasciitis is, “will it hurt?” The answer, of course, depends on the type of therapy you and your physical therapist choose. However, in general, guided stretching and exercises shouldn’t hurt. You may feel some discomfort as you stretch and strengthen damaged and weak muscles and ligaments, especially during the postoperative period, but there’s no need to brace yourself for severe pain.

That said, communication is very important. While your physical therapist is a trained professional, he or she isn’t a mind reader. If something hurts or feels wrong, don’t be shy about speaking up. Let your physical therapist know, so your position or treatment can be adjusted properly.
The other big question many people have about what to expect from physical therapy is “how long will it take?” or “how many sessions will I need?” Again, the answer depends a great deal on a few factors, including how long you have been dealing with plantar fasciitis, whether or not you are recovering from surgery, your particular body and other coexisting conditions, and how diligent you are about supplementing in-office physical therapy with at-home treatment. Physical therapy can be a process of as little as a few weeks, or many months, depending on your unique situation.
Physical Therapy Costs
The cost of physical therapy for plantar fasciitis depends on a combination of the following factors:
- Number of sessions you need
- The complexity of the problem, including other conditions you’re dealing with simultaneously
- The therapist you choose and his or her treatment plan
- How much you’re able–and willing–to supplement your physical therapy with at-home exercises and activities
- Whether or not your physical therapy sessions are covered by insurance
Expect to pay anywhere from $10-$75 per session, with insurance, and between $50-$350 per session without insurance. Smaller practices are often less expensive and may be a good place to start if you don’t have insurance. You’ll also want to plan for costs that may arise throughout the course of your physical therapy, based on recommendations by your physical therapist such as night splints, orthotics for plantar fasciitis, and heel wraps.
Common Physical Therapy Stretches and Exercises
Your physical therapist will work with you to create a specialized treatment plan. He or she will guide you through stretches and manual therapy like massage to help strengthen and improve flexibility in the arch and its supporting muscles and tendons. Here are five of the most common types of exercises and stretches you’re likely to encounter in physical therapy. With a little creativity, you can also perform these types of stretches at home:
Arch stretches:
Stretches that improve strength and flexibility of the arch are critical to physical therapy since the arch is the weight-bearing mechanism that has become compromised through plantar fasciitis. Your physical therapist will guide you through stretches that engage, lengthen, and improve circulation in this vital ligament.
At-home support: Stretch your arch using a simple water bottle or tennis ball.
Toe stretches:
Exercises that strengthen the toes will also build strength and flexibility in the muscles and ligaments throughout the foot. Your physical therapist may guide you through stretches to grab small objects or grasp with your toes.
At-home support: Strengthen your toes by grasping for pebbles or marbles.
Ankle mobility stretches:
Limited ankle mobility can play a factor in plantar fasciitis since an inflexible ankle impedes the arch from absorbing impact properly. Your physical therapist may use stretches designed to help you improve the range of motion and flexibility in your ankles.
At-home support: Use a staircase stretch to build and improve ankle mobility.
Achilles tendon stretches:
A tight Achilles tendon can lead to gait abnormalities that take a serious toll on your arch. Your therapist may use stretches designed to lengthen and loosen a tight Achilles tendon to help improve your gait.
At-home support: The wall and book stretch help strengthen and stretch the Achilles tendon.
Calf stretches:
The calves can become tight and limited in proper function either in response to plantar fasciitis or as a contributing cause of plantar fasciitis. Your physical therapist may work on stretching and lengthening your calves to allow your legs and feet to work together properly.
At-home support: Wall squats can help lengthen and stretch the calves at home.
In addition to asking you to supplement your physical therapy at home with stretches for plantar fasciitis, your physical therapist will likely encourage you to continue conservative, at-home treatment options. These tried-and-true treatments can support and improve the effectiveness of your in-office physical therapy and include wearing orthotics, icing as needed, resting as much as possible, and using NSAIDs for pain and inflammation as needed.
Physical therapy can be an incredibly helpful resource for recovery and support, especially for difficult-to-treat cases of plantar fasciitis, or after surgery during the healing process. With the right physical therapist on your side, your journey toward healing can be expedited and improved.
Common Physical Therapy Treatments
| Ultrasound | Graston | TENS Therapy |
| Laser Therapy | Osteopathic Manipulative Treatment | Soft Tissue Mobilization |
| Dry Cupping | Cryotherapy | Active Release Technique |
Can Orthotics Improve Posture?
 “Posture” simply means the way you hold your body while sitting or standing. But the complex combination of muscle groups and other body tissue involved in creating healthy posture is a little more complex, involving nearly every muscle group in the human body including the neck muscles, abdominals, back muscles, leg muscles, and feet.
“Posture” simply means the way you hold your body while sitting or standing. But the complex combination of muscle groups and other body tissue involved in creating healthy posture is a little more complex, involving nearly every muscle group in the human body including the neck muscles, abdominals, back muscles, leg muscles, and feet.
While the body’s “core” tends to get the spotlight when it comes to good posture, one of the most significant–but often overlooked–contributors to good posture is the feet and arches.
Which raises the question: Can orthotics–which support the feet and arches–improve posture?
In this article we’ll explore why good posture is important to your overall health, and whether orthotics can help you gain the benefits of good posture.
Overall Health Benefits of Good Posture
In Western culture, good posture is often seen as just a sign of a cultured, refined person. However, the recognized benefits of good posture go much deeper than propriety.
When the body’s muscle groups, ligaments, tendons, and bones are working together properly while sitting or standing, each group is able to work more effectively individually and as a whole. Good posture can improve overall blood circulation and can also reduce strain, aches and pains to the neck, shoulders, back, and hips.
Healthy posture is also critical for reducing and minimizing the amount of wear and tear placed on joints and fascia throughout the body. Additionally, it helps avoid atrophy and overuse of different muscles throughout the body, since muscles are being engaged properly and in cohesion.

Postural Benefits of Wearing Orthotics
Wearing orthotics can have a tremendous positive impact on good posture, since the way the feet absorb and distribute impact has a big effect on the rest of the body. While orthotics are often seen as just a solution for heel pain, they can also be used as simple at-home solution to improve posture in the following ways:
Correct Gait Abnormalities
Your feet are your foundation every time you run, walk, jump, or stand. The impact from these simple daily activities, combined with the weight of the human body can place a great deal of strain on the heel and arch of the foot. Over time, as the body tries to compensate for this strain and pain, gait abnormalities can develop that result in poor posture.
Improve Balance

Since orthotics help lift the arch to an optimal height and cushion the heel, the feet (and therefore the ankles, legs, hips, etc.) are more balanced, helping you avoid stumbles and falls that can injure or throw any number of the body’s muscle groups, bones, or tissues out of alignment and creating poor posture.
Reduce Pronation
Pronation is where your foot turns too far inward as you step forward, causing the arch to flatten excessively. Pronation is associated with increased incidences of plantar fasciitis, heel pain, gait abnormalities–and poor posture. Orthotics can help correct overpronation while you walk.
Distribute Weight and Impact More Effectively
Because orthotics cushion and support the arch, you’re able to more effectively distribute and bear the weight of walking, running, and jumping. And when your arch is able to do its job in absorbing impact effectively, you’ll feel less aches and strain to your hips, back, and legs.
What to Look for in Orthotics to Improve Posture
There are a lot of different orthotics to choose from on the market. If you’re looking to improve your posture, you’ll want to keep an eye out for the following qualities:
Lightweight: Heavy orthotic shoes can negate some of the positive postural effects of using orthotics in the first place, and don’t allow for much flexibility in rotating between different pairs of shoes. Look for lightweight orthotic inserts that can be added to any pair of shoes.
Cost effective: There’s not much evidence that expensive prescription orthotics are any more effective than inexpensive orthotic inserts (some of which are more than 90% effective in treating heel pain and plantar fasciitis!) Balance quality with cost!
Cushioning and Supportive: The perfect blend of support and cushioning can be surprisingly hard to find. If you can crush your orthotic insert in your hand, it’s not likely to stand up very well to the rigors of walking, running, or jumping. Make sure your chosen orthotic is sturdy enough to stand up to some pressure while still providing cushioning for your heel and arch.
Fascia Bar Technology: This patented technology brings the arch to the optimal height for support and comfort during physical activity. This innovative technology helps the arch tremendously with weight distribution and impact absorption.
There’s no question that posture is important. And there’s little doubt that the right pair of orthotics can help you reap the benefits of healthy posture by keeping your gait, balance, and ability to absorb impact properly on point.
 |
|
|---|
Plantar Fasciitis and Martial Arts
 Youth and adults alike enjoy martial arts for good reason. With numerous popular martial arts disciplines, there’s something for every ability, style, and age group. And not only can martial arts improve flexibility, muscle control, strength, and cardiovascular health; many disciplines offer mental health benefits including a constructive outlet for stress or anger, meditation techniques, mental control, and stress reduction.
Youth and adults alike enjoy martial arts for good reason. With numerous popular martial arts disciplines, there’s something for every ability, style, and age group. And not only can martial arts improve flexibility, muscle control, strength, and cardiovascular health; many disciplines offer mental health benefits including a constructive outlet for stress or anger, meditation techniques, mental control, and stress reduction.
Many people with plantar fasciitis have found that low-impact martial arts disciplines can be an ideal form of exercise that doesn’t aggravate their heel pain. However, just as many martial artists have developed plantar fasciitis and heel pain as a direct result of their involvement with martial arts.
Choosing a martial arts discipline wisely, preparing for your class or match properly with the correct gear, and knowing how to recognize and treat heel pain can mean the difference between a long and healthy career in the martial arts, and high risk of injury to the feet and heels.
Choosing a Martial Arts Discipline with Foot Health in Mind
If you have previously or are currently dealing with heel pain and plantar fasciitis, choosing a martial arts discipline is extremely important to avoid aggravating heel pain or relapsing. The higher impact (think kicks, strikes, and jumps), the longer the durations of standing, and the type of flooring you’ll be practicing on are all important factors.
You’ll also want to consider your relationship with your instructor and his or her flexibility. Most instructors are happy to allow you to modify or accommodate specific health concerns. Make sure you’re comfortable communicating your needs with your instructor.
If you have a history of plantar fasciitis, you may want to avoid very high impact martial arts disciplines that rely heavily on foot strikes like muay thai, taekwondo, hapkido, and karate. Low impact, gentler disciplines that emphasize wrestling, groundwork, and upper body work, like jiu jitsu, tai chi, or chi gong.
If your heels and feet are pain-free, and your arches are healthy, you may choose to engage in a higher-impact form of martial arts. However, you’ll want to take extra care to wear the proper gear and notice and treat any signs of plantar fasciitis.
Proper Gear and Support for Martial Arts

The proper gear and support are critical for a long and healthy career in any discipline of martial arts, whether or not you currently suffer from heel pain:
Footwear: While some instructors and disciplines encourage barefoot work, be extremely cautious of this approach–especially in high-impact martial arts disciplines that involve kicks, jumps, and strikes. These moves can place a great deal of strain and pressure on the arch of the foot, leading to small tears and progressive injury. Wear lightweight, supportive footwear with arch supports when possible. When going barefoot is required or preferable, wrap your feet with barefoot heel wraps, which drastically improve arch support while allowing for the flexibility and feel of bare feet.
Practice Surface: While a hardwood or laminate floor may look professional and is easy to keep clean after all those bare feet, this surface is very hard on feet and arches. When possible, practice on a mat or other supportive but cushioning surface. When in doubt, ask your instructor. He or she may have mats available for use.
Proper Warmup: Don’t underestimate the importance of stretching your feet and legs prior to a practice or competition, no matter which discipline of martial arts you choose. Take the time to stretch your calves, Achilles tendon, toes, and arch each time. This will help your feet and supporting tissue flex and stretch appropriately rather than succumbing to injury or strain.
Ongoing Muscle Strengthening: If you’re dedicated to avoiding injury to your feet in the martial arts, you should know that stretching and muscle strengthening can be used very effectively on a daily basis in addition to warm-up sessions. Not only will you avoid injury–you’ll notice improvements in your flexibility and capability in your chosen discipline.
Proper Rest Between Sessions: As with any exercise or activity, don’t push yourself too hard, especially when you’re just getting started. Build your muscles and allow them to rest properly in between. While it can be thrilling to learn a new skill or practice, allowing your muscles and ligaments proper rest will help build your tolerance for a new activity.
Recognizing and Treating Symptoms of Plantar Fasciitis from the Martial Arts

Plantar fasciitis and heel pain may onset suddenly or gradually over time. You’ll want to pay close attention to any of the following symptoms:
- Pain that is worst first thing in the morning as you step out of bed, and gradually improves throughout the day
- Dull or aching pain and/or stabbing “needle-like” pain with each step, in one or both feet
- Redness or inflammation along the bottom of the foot
- Swelling in the affected foot
If you notice any of these symptoms, it’s important to take appropriate action to head off plantar fasciitis early. At-home remedies for heel pain and plantar fasciitis are extremely effective, especially when used promptly:
- Use NSAIDs (non-steroidal anti-inflammatories) like Ibuprofen to reduce swelling and manage pain
- Ice your feet as needed to reduce swelling and inflammation
- Use orthotic inserts whenever possible to support and cushion your compromised arch
- Rest your feet as much as possible to allow your arch to heal
- Stretch your feet and arch to improve strength and flexibility
- Evaluate whether you are maintaining a healthy weight, and take steps to lose weight if needed.
- Obesity is highly linked with plantar fasciitis because of the additional impact extra weight puts on the arches.
By informing yourself about the right martial arts discipline for you, the proper gear to support you in your pursuit, and staying proactive about symptoms of plantar fasciitis, you can avoid heel pain and enjoy all the mental and physical benefits that the martial arts can provide.