Why Did My Feet Start Hurting When I Turned 50?
Walking on Broken Glass
I’d always taken a lot of pride in staying active. When I was a younger woman, I ran half marathons. As I got older, I slowed down a little but I still regularly played tennis and hiked in the foothills near my home. I’d had sore feet before — nothing major. But I’d never experienced anything like the “walking on shards of glass” feeling that made the first steps out of bed in the morning almost unbearable. I stopped playing tennis, stopped hiking, even stopped walking to the mailbox when I could avoid it, because my feet hurt so much. In a panic, I made an appointment with a podiatrist.Learning I’d Lost the Spring in My Step
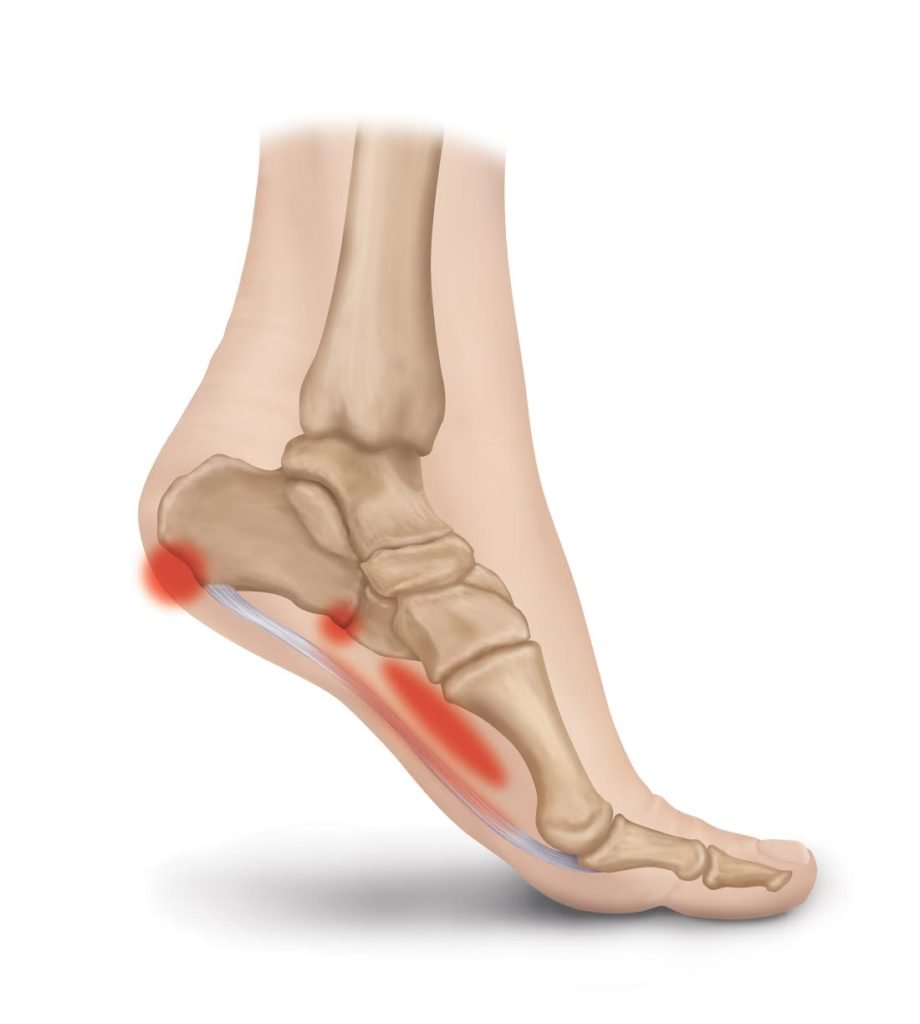
At the podiatrist’s office, there was good news, and there was bad news. The bad news came first: I had literally lost the “spring” in my step. After listening to my symptoms and doing some imaging to rule out a stress fracture, the doctor explained that I had a condition known as “plantar fasciitis.” He explained that the plantar fascia is the “springy” ligament that runs from the heel to the ball of the foot, and helps absorb impact. Those “springs” can wear out as a result of injury, overuse— or the normal aging process. My doctor explained that while athletes are the ones who make news headlines when they get plantar fasciitis, the most common risk factor for the condition is age! And that wasn’t all:And Bunions, Too!
It turned out that plantar fasciitis wasn’t my only problem. I also had bunions (which may have been a contributing factor in my plantar fasciitis). I’d notice that the bump where my big toes met my foot seemed to be more pronounced than my husband’s — and I could feel it rub against my shoes while I walked. Sometimes, after a tennis match, I realized they were red and inflamed. But I didn’t know that bunions could subtly change my gait over time and strain my arch as my body tried to minimize the discomfortOkay, How Did This Happen to Me?
My podiatrist reassured me that aging feet are simply at higher risk for different conditions that cause foot pain — including plantar fasciitis. The doctor reassured me that while the bunions and my active lifestyle might have played a role in my plantar fasciitis diagnosis, age was likely the main contributing factor. I had no idea that the aging process flattens and widens the feet, making it harder for the plantar fascia (that spring in my step) to absorb impact, and wearing down the heel’s natural fatty cushioning. Older adults also deal with changes in circulation (which may slow healing when we overuse or injure our feet), and changes in the strength of skin and tissue that make injuries from rubbing or pressure more common (hello, bunions!).Finding Answers for Foot Pain
My doctor was quick to reassure me that foot pain wasn’t a life sentence. I was also relieved to learn that most people with a diagnosis of plantar fasciitis recover within a few months — without surgery. I left the podiatrist’s office with a prescription for rest, stretching exercises for my plantar fascia, and instructions to ice my feet whenever they felt inflamed or painful. My doctor also recommended orthotic inserts that I could slip into almost any pair of shoes I already owned, to help support my injured arch and make walking much less painful. I was given strict instructions to stop wearing shoes that rubbed against my feet while I walked, or were too tight in the toes.Getting My Spring Back!
I’m happy to say that while I might be “over the hill,” I’m back to hiking in the hills without foot pain! It took a few months. And I’m more vigilant about giving my feet a good rest after a long hike than I was before. But it’s safe to say I have the spring back in my step. Those orthotic inserts my podiatrist recommended were a lifesaver. In the short term, they took the pressure off my arch and relieved that “walking on broken glass” sensation. And in the long term, combined with stretching to improve my strength and flexibility, and better-fitting shoes, my arch actually was able to heal and recover. I’ve also added the following tools into my daily and weekly routine. After learning what it’s like to be knocked off my feet, I’m doing everything I can to keep them healthy:- Orthotic inserts: My doctor recommended fascia bar inserts because they are more effective than regular cushioning and arch support
- Compression socks: These socks help improve my blood circulation, important for older adults
- Massage ball: This little ball helps roll out painful muscle knots and scar tissue, as well as improving circulation in my feet
- Ice therapy slippers: Since I ice my feet regularly, I wanted an upgrade from the ziploc bag! These slippers stay in place, with no mess, and strap right to your feet.
Can Uric Acid Cause Heel Pain? Signs of Gout in the Heel
 The word gout comes from the Greek word podagra, which literally translates to “foot grabber.”
The word gout comes from the Greek word podagra, which literally translates to “foot grabber.”
Gout is a type of arthritis caused by a buildup of uric acid and characterized by foot pain, swelling, redness, and difficulty walking is typically localized in the big toe. However, some types of gout may be localized in the heel, making it difficult to distinguish from plantar fasciitis.
Let’s explore the connection between gout and heel pain, as well as symptoms that can help you tell the difference between plantar fasciitis and gout
The Connection Between Heel Pain and Gout
While it’s fairly rare for gout pain to appear in the heel (instead of near the big toe), it does happen!
Gout that leads to foot pain develops when there are high levels of uric acid in the body. And high levels of uric acid are most likely to develop under the following conditions:
- Diet: A diet that is heavily focused on red meat, sugar (particularly fructose), and alcohol (beer, in particular) can increase levels of uric acid and gout.
- Increase in body fat: As your body increases its stores of body fat, uric acid levels rise, and your kidneys may struggle to eliminate the excess.
- Medications: Some medications, including hypertension, may increase uric acid in the body. Studies show that Thiazide diuretics (which treat hypertension) are key culprits.
- Untreated medical conditions: High blood pressure, metabolic syndrome, diabetes, and kidney disease can all contribute to higher than usual levels of uric acid in the body, and gout.
- Genetics and gender: There is a genetic link to gout. If you have a family history of gout, you may be especially susceptible. Younger men are more likely to get gout than women; however, postmenopausal women have an increased risk as well.
How Can High Uric Acid Cause Heel Pain?
So, why does gout show up in the feet (as opposed to other body parts)? Uric acid is very sensitive to cooler temperatures. As it circulates throughout the body and reaches the feet (furthest from the heart and typically the coolest), the liquid uric acid crystalizes, leading to pain in the joints of the big toe or joint of the heel (where the heel bone meets the ankle bone).
Uric acid levels rise when your body breaks down “purines.” Purines are found in foods like red meat and alcohol, as well as in certain medications and naturally in the human body (especially as fat stores increase).
Most of the time, your body is able to manage uric acid levels effectively, simply dumping the uric acid into your kidneys where it is excreted as urine. However, when uric acid levels get high enough, your kidneys may struggle to keep up, and uric acid may stay in your bloodstream where it causes inflammation, pain, and swelling as it crystallizes in the joints of the foot.
Is My Heel Pain Gout or Plantar Fasciitis?
Heel pain can be confusing at times. While the most common cause of heel pain is plantar fasciitis, other less common ailments like gout can mimic similar symptoms! Use this helpful symptom guide to determine whether you’re dealing with plantar fasciitis or gout:
Symptoms of Heel Pain from Plantar Fasciitis
The hallmark symptoms of plantar fasciitis include the following:
- Heel pain that’s most intense first thing in the morning (when the plantar fascia hasn’t “warmed up” yet through movement).
- Pain that improves somewhat with stretching and low-impact physical activity
- Sharp or dull pain, accompanied by redness or swelling
- Pain that coincides with weight gain
- Difficulty walking or standing on the affected foot (plantar fasciitis can happen in both feet, though more rarely!)
- Pain that improves through the use of orthotics that help properly realign and cushion the plantar fascia
Symptoms of Heel Pain Due to Uric Acid
Anyone can get gout, although it’s most common in individuals with the risk factors we covered earlier (like heavy alcohol use, or a diet that includes a lot of red meat.) The symptoms of gout in the heel are subtly different from those of plantar fasciitis in the heel:
- Redness, swelling and tenderness that is most pronounced where the heel meets the ankle. You are also likely to notice symptoms at the base of the big toe.
- Often, gout symptoms will flare-up in the middle of the night (when that uric acid settles and cools during this period of low activity)
- During a flare-up, your heel will feel so hot and painful to the touch that even wearing socks is excruciating
- Pain that is less intense but lingers after a “gout attack” flare-up of pain
- Increasing difficulty moving the joint
As a general rule of thumb, pain from plantar fasciitis will improve with rest, while pain from gout will flare up during long periods of inactivity and rest.
Treating Heel Pain from Gout
Thankfully, most cases of heel pain from gout can be successfully resolved with minimal medical intervention and changes to diet and lifestyle.
Medications
NSAIDs (non-steroidal anti-inflammatory drugs) like Tylenol and Ibuprofen can help relieve pain from a gout attack, as well as reduce pain and swelling in the heel.
Colchicine is another common medication prescribed to treat pain from gout, however, it can cause severe side effects like nausea and diarrhea. Your doctor will likely recommend the minimal dose needed.
Corticosteroids are used in rare cases when NSAIDs or Colchicine can’t be taken since these drugs have serious side effects including high blood pressure and high blood sugar.
If you have ongoing gout attacks, or severe ongoing gout symptoms your doctor may also consider prescribing medication that limits the amount of uric acid your body produces.
Lifestyle Changes
Limit foods that increase uric acid production: These foods include alcohol, red meat, seafood, organ meats, fructose sugars, and other foods high in purines.
Exercise and manage weight when possible: As possible, maintain a healthy weight to keep the body’s own production of uric acid down.
Drink coffee: While scientists don’t understand the link completely, some studies have shown that drinking coffee can help lower your levels of uric acid!
Add more vitamin C to your diet: Taking at least 500 mg of vitamin C each day (and eating foods rich in vitamin C) has been shown to make a measurable, positive impact on uric acid levels in the body!
Have you suffered from heel pain that turned out to be gout? Tell us about your experience in the comments below!
What Causes Pain on the Inside of the Heel?
 No matter where heel pain strikes (front, middle, back, or everywhere!), the biggest question on your mind is likely, “How can I make it stop?” However, the location of your heel pain reveals important clues about its underlying cause!
No matter where heel pain strikes (front, middle, back, or everywhere!), the biggest question on your mind is likely, “How can I make it stop?” However, the location of your heel pain reveals important clues about its underlying cause!
Inner heel pain can present as achy, bruise-like, or sharp and intense. By understanding your unique symptoms and honing in on the why your inner heel hurts, you can take more effective steps toward treatment. Let’s get to the bottom of your inner heel pain:
Why Does My Inner Heel Hurt?
The most common causes of heel pain deep within the heel are trapped nerves, plantar fasciitis, fat pad syndrome, and stress fractures.
Trapped Nerves in the Heel
Sometimes, nerves in the heel can become “entrapped,” or squeezed/constricted because of injury to the foot, trauma, or simply overuse. There are several key nerves that run along the inside of the heel and connect to the posterior tibial nerve. These nerves include the medial plantar nerve medial calcaneal nerve, the lateral plantar nerve, and the nerve to the abductor digiti minimi.
Telltale Symptoms
- Pain may feel tingling, numb, or burning
- You may notice tenderness to the touch along the inner heel. The exact location of the pain will depend on which nerve is entrapped.
- Symptoms may flare up when you walk or participate in physical activities, and improve somewhat with rest
- Pain from an entrapped nerve is usually felt in just one foot
Treatment Options
If your inner heel pain is caused by an entrapped nerve, your doctor will likely recommend rest from activities that aggravate pain, icing, stretching, and anti-inflammatory medication as needed. If these more conservative treatment methods do not work, your doctor may recommend surgery to decompress the entrapped nerve.
Heel Pad Syndrome
A thin, atrophied heel pad can result in a painful condition known as Heel Pad Syndrome. This condition can be caused by aging, weight gain, repetitive impact on hard surfaces, or unsupportive, uncushioned footwear.
Telltale Symptoms
- Bruise-like pain deep in the heel as the fat pad is no longer able to cushion the heel effectively
- Pain that can be recreated by firm pressure on the bottom of the heel
- Pain that gets worse when you walk on hard surfaces
- Heel Pad Syndrome is often closely linked with plantar fasciitis
Treatment Options
Treatments for Heel Pad Syndrome involve lots of rest and better support and cushioning for the heel. Your doctor will likely recommend icing, anti-inflammatory medicines as needed, taping, and orthotic inserts that cushion the heel, support the foot, and reduce pain while walking.
Stress Fractures on the Heel
A stress fracture on the heel is a very thin crack in the heel bone that can be caused by repetitive stress or impact to the heel, or a sudden blow to the heel. The risk for stress fractures is elevated in high impact sports, for people with osteoporosis or with low vitamin D levels, or for individuals who increase the intensity of their workouts significantly without warming up.
Telltale Symptoms
- Pain may come on gradually or onset suddenly and is typically sharp and intense
- Pain that gets worse the longer you stay on your feet and gets worse if you stretch
- Pain that is located in one very specific spot on the heel
- Swelling, redness, and tenderness to the touch
Treatment Options
It’s important to see a doctor and treat suspected stress fractures right away, to avoid further damage or a complete break in the bone. Your doctor may recommend an Ace Bandage or KT tape to help stabilize the foot, and may also recommend crutches, a cast, and complete rest from the foot while you heal. Icing and anti-inflammatories can help with pain while you heal.
Plantar Fasciitis
Plantar fasciitis is caused by damage to the plantar fascia ligament, which runs from the heel to the ball of the foot. This damage, combined with inflammation in the heel can lead to intense pain in the heel. Risk factors for plantar fasciitis include weight gain, wearing unsupportive shoes, intense exercise without proper warmup, and jobs that require a lot of standing and walking.
Telltale Symptoms
- Pain that is worst in the morning, with the first few steps out of bed
- Pain that gets slightly better with movement and improves with stretching
- Stiff, aching heels
- Swelling, pain, and inflammation in the heels
- Pain may be dull, or sharp and needling
Treatment Options
Thankfully, most cases of plantar fasciitis can be treated at home with rest, stretches to improve flexibility, and orthotic inserts that realign the plantar fascia and cushion the heel. Icing, anti-inflammatory medication, and dietary changes to lose weight when possible can also help speed up healing.
What to Do if You Have Inner Heel Pain
If you have inner heel pain, the most important thing you can do is hone in on your unique symptoms and educate yourself — while you rest from any activities that seem to be exacerbating the pain!
This information will help you communicate effectively with your doctor, determine the source of your inner heel pain, and form an effective and actionable plan for treatment.
In general, most cases of inner heel pain can be resolved with conservative treatment rather than invasive medical procedures like surgery. Unless your heel pain is very severe, or you suspect a fracture, try conservative treatment methods first! In most cases, you’ll be back on your feet in a relatively short amount of time.
16 Products to Melt Away Foot Pain — Fast
Wondering which foot pain products are the real game-changers for heel pain or plantar fasciitis?
You won’t find any so-so or “it worked okay” products on this list. Every single one is a slam dunk (a most have a money-back guarantee to boot!)
Just so you know, we participate in the Amazon Affiliates program, so we may earn a small commission if you purchase through the links in this article.
1. Heel Seats
It’s no surprise that so many people have nicknamed these orthotic inserts “Little blue miracles.” Skeptical? Just read the thousands of glowing reviews from plantar fasciitis sufferers who thought they had tried “everything” for foot pain.”
Not only do washable, reusable Heel Seats hold their shape time after time (unlike the cheap foam ones that end up crushed and flat), but they provide just the right amount of support, combined with just the right amount of cushioning. Most people notice a difference in pain relief right away, and after a few weeks of wear you can expect to kiss foot pain goodbye — or your money back.
Click here to get Heel Seats (add two pairs to your cart for a special discount!)
2. Anti-Inflammatory Cream
Penetrex was developed in Southern California after eight years of research. And this stuff is a lifesaver for quick foot pain relief. It won’t stain your socks, won’t leave your feet feeling slippery or greasy, and it doesn’t have a weird smell (which makes it especially great for the office or on the job!).
Bonus: It also comes with an unconditional guarantee: “Pain-free results, or a pain-free refund.”
Click here to get Penetrex inflammation cream.
3. Barefoot Wraps
Move aside, flip-flops. There’s no need to choose between adorable (but flimsy and unsupportive) footwear for the beach, and stodgy, hot orthotic shoes. Heel Seat Wraps can be worn with almost any pair of sandals (or all by themselves!) for summery, toes-in-the-sand bliss combined with arch support and pain relief.
Click here to get barefoot wraps.
4. Yoga Toes
If hammer toes or bunions are the cause of your foot pain, a toe stretcher like Yoga Toes can make a world of difference!
Toe separators gently uncurl, separate, and stretch, painful or deformed toes while you rest, improving circulation, realigning the toes, and gently stretching the tendons and muscles of the foot. This can also be beneficial for heel pain and plantar fasciitis!
5. Ice Therapy Slippers
These slippers are an absolute game-changer when it comes to icing your feet. No more Ziploc baggies of leaking, watery ice cubes (that freeze into crazy shapes when you try to reuse them!).
Ice Therapy Slippers are foot-shaped ice packs that strap right to your feet, so they stay put, delivering soothing cold therapy to inflamed, painful heels or feet. When you’re done icing, just pop them back in the freezer for next time!
Click here to get Ice Slippers.
6. Foot Stretcher
Let’s face it: It’s not always easy to get that perfect stretch for your arch. The no-slip ProStretch foot stretcher allows you to get a deeper, perfectly positioned stretch that can help loosen tight calves, heels, arches, and hamstrings; improve strength and flexibility; and improve blood flow.
Click here to get the ProFoot Stretcher.
7. KT Tape
A damaged, injured plantar fascia needs stability and support. Taping up the foot and arch with KT tape is a fantastic way to help stabilize the plantar fascia and limit movement while you heal. The extra compression and support is also a lifesaver for pain relief!
There’s a slight learning curve when it comes to taping technique, but the good news is that tape can stay put for several days (and overnight!) before it starts to peel off.
Click here to get Kinesiology Tape.
8. Compression Socks
Hold on, don’t skip this one! You might think you’ve tried compression socks before, but if you haven’t tried these babies, you haven’t tried compression socks! With gentle yet firm compression, comfortable cuffs, and roomy toes you’ll feel supported–without feeling strangled! The material is breathable, anti-fungal, and cozy. Wear them day or night for soothing compression that helps reduce swelling and promote blood circulation.
Click here to get compression socks.
9. Calf/Foot Massager
Speaking of circulation, this calf/foot massager is a true gem that improves circulation soothes aching feet. Give yourself the gift of the perfect foot/calf massage every single night! The slip-on boots have two massage modes, with three intensity levels and a handheld remote control. (Don’t be too surprised if you spouse or roommate tries to steal this one!)
Click here to get the foot and leg massager.
10. Foot Massage Ball
A massage ball made especially for plantar fasciitis is just the ticket for anytime pain relief. Pop it in your purse, desk drawer, or even in your glovebox! Just roll it along the bottom of each foot for 2-3 minutes to help relieve tightness and knots, improve blood flow, and relieve pain quickly.
Click here to get a foot massage ball.
11. Metatarsal Pad
If your foot pain is localized in the metatarsal area (where the toes connect to the foot) from diabetes, Morton’s neuroma, calluses, or bunions a metatarsal pad can be a lifesaver. This soft gel pad cushions and compresses the ball of the foot for pain relief, support, and help properly distributing bodyweight while walking and other physical activities.
Click here to get metatarsal pads.
12. Plantar Fasciitis eBook
Knowledge is power–and one of the most important ways you can beat foot pain! This free plantar fasciitis ebook covers causes and symptoms of plantar fasciitis, as well as proven natural and medical treatment options for foot pain!
Click here to get the free plantar fasciitis ebook.
13. Tens Machine
While electrical current might sound like a strange solution for foot pain, it’s actually pretty incredible. A tens machine delivers an “electrical massage,” using sticky electrodes that attach to your foot. These low-voltage pulses help stimulate the muscles for better blood circulation, reduced inflammation, and rapid temporary pain relief.
Click here to get a tens machine.
14. Cupping Set
Cupping is standard practice for injured athletes— and if you’ve ever wondered what you might be missing, this cupping set is an excellent option! Cupping can help improve foot pain through a unique deep-tissue massage as the cups pull the skin and tissue of the foot into the vacuum created by the cups.
Click here to get the cupping set.
15. Full-Length Arch Supports
If you have foot pain paired with high arches, standard orthotic inserts might not cut it. Full-Length Heel Seats take support to the next level, by gently cradling the entire foot while re-aligning the arch to an ideal position.
Click here to get Full Length Heel Seats.
16. Heated Foot Warmer
You know that “ahhh” feeling when you step into a perfectly warm bath? This soft, heated foot warmer is like that! Use it to relieve muscle aches, relax and warm cold feet, and stimulate blood flow in painful feet.
The Consequences of Leaving Plantar Fasciitis Untreated
First, the good news: 90% of plantar fasciitis cases can be successfully resolved with simple, conservative treatments.
What’s the bad news? The longer plantar fasciitis goes unaddressed, the longer the healing process takes and the more potential complications that may arise. Not allowing your arch enough rest time after a foot injury, working a job that requires a lot of time on your feet, participating in high-impact activities without proper footwear or support, and failing to follow through with at-home treatments after symptoms develop are the most common ways plantar fasciitis persists and gets worse.
Click here to get the #1 plantar fasciitis inserts.
Risks of Untreated Plantar Fasciitis
Symptoms of plantar fasciitis and heel pain usually develop gradually, although some cases can develop more quickly (for instance, after a foot injury). If heel pain and other symptoms of plantar fasciitis (like redness, inflammation, and swelling in the feet) are left untreated, other more serious complications can arise:
Plantar Tears
Over time, if plantar fasciitis is left untreated, the inflammation and stress to the plantar fascia can result in small tears in the fascia (sometimes called “micro-injuries”). You may not be aware of the exact moment that each small tear appears, however you will notice your pain level gradually worsen. If these tears are left unaddressed, they may grow in size and number, and make the plantar fascia more vulnerable to rupture and debilitation.
Plantar Rupture
Plantar rupture can happen if plantar fasciitis is not addressed, but an individual continues to participate in activities that place a great deal of impact on the plantar fascia. These activities might include jogging, sports, or even standing for long periods of time in ill-fitting footwear.
Symptoms of plantar fascia rupture usually include a loud popping sound, followed by intense pain, bruising, and swelling in the foot. Putting weight on the affected foot will be very painful. If you suspect plantar rupture, you should seek medical help immediately. You will likely be required to wear a boot or crutches for a period of time after a ruptured plantar fascia.
Research also shows that steroid injections, a common treatment for pain relief of chronic plantar fasciitis, are a significant risk factor for plantar rupture, because of the way that the steroids interfere with collagen synthesis in the foot.
Plantar Fibromatosis
Plantar fibromatosis is a condition in which benign, slow-growing nodules form along the plantar fascia. The nodules often grow slowly and undetected, followed by sudden, rapid growth. As time passes and the nodules grow, walking may become uncomfortable or painful.
While many cases of plantar fibromatosis are believed to be triggered by genetics, there is is a correlation between individuals with plantar fasciitis and individuals with plantar fibromatosis. Some researchers believe that plantar fibromatosis can be triggered by a tear in the fascia that is left untreated.
Heel Spurs
Heel spurs are one of the most common consequences of leaving plantar fasciitis untreated. In an attempt to protect the arch of your foot and mitigate damage, your body sends an army of cells to the site of the problem, which begins depositing calcium. Over time, these deposits can build up into sharp protrusions that dig into the fatty pad of the heel and cause a great deal of pain with each step.
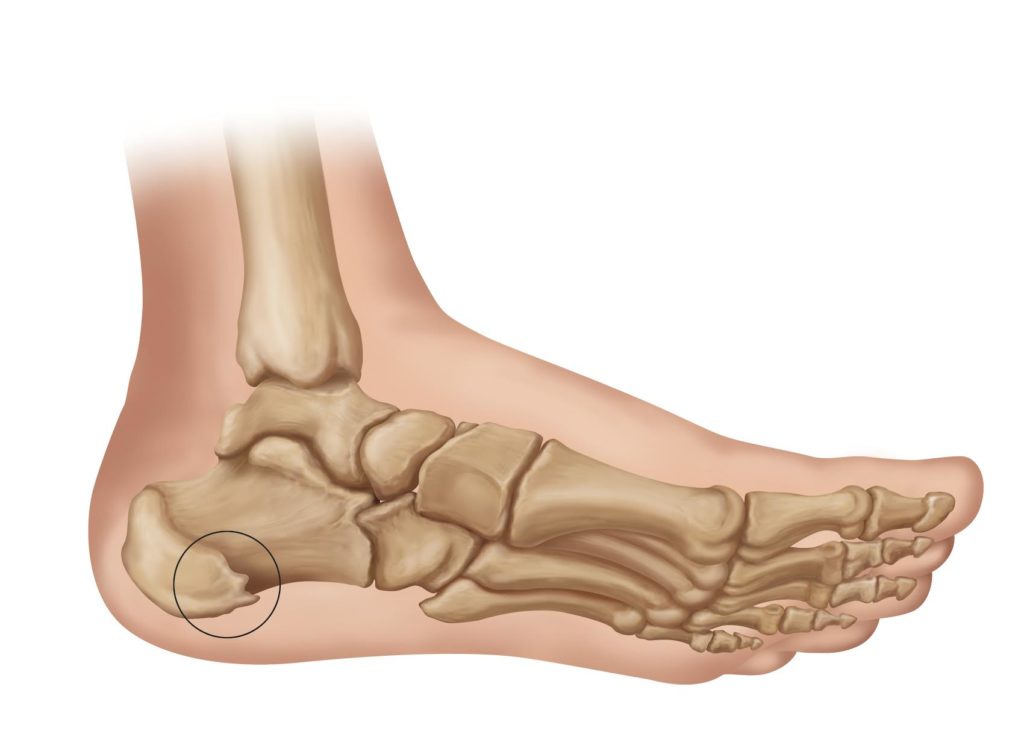
Heel spurs can build up over several months’ time without causing pain. In other words, allowing plantar fasciitis to go untreated may mean that a secondary problem brews unnoticed–until the sharp pain reappears.
Complicated Decisions About Surgery and Medical Interventions
Left untreated, plantar fasciitis can become chronic and make surgery more likely. While surgery can be a successful last resort for cases of chronic plantar fasciitis that don’t respond to conservative treatments like orthotics, rest, and icing, it’s important to remember that surgery can often be avoided through prompt and consistent treatment when heel pain arises.
Help avoid complicated (and expensive) decisions about surgery and other medical interventions by taking symptoms of plantar fasciitis seriously!
Hip, Knee, and Back Pain from Plantar Fasciitis
Over time, untreated plantar fasciitis and heel pain can lead to unexpected hip, back, and knee pain. The arches of the feet work in tandem with the tendons, ligaments, and muscles throughout the lower body. When the plantar fascia is compromised, other muscles, ligaments, and tendons must work harder to compensate. This cascade of overuse can eventually lead to pain outside the arch.
Plantar fasciitis can also lead to abnormal gait patterns while walking or standing, leading to repetitive stress injuries as the hips, knees, and backs are repeatedly required to move in abnormal ways.
Listen to the Warning Signs of Plantar Fasciitis
Recognizing the symptoms of plantar fasciitis and treating this condition early is the best way to avoid secondary problems and complications. Think of the pain from developing plantar fasciitis as a warning, encouraging you to address the problem at hand before more damage occurs. Stretching, icing, and using special orthotic inserts are all effective ways to curb the damage from plantar fasciitis and begin healing.
This article was originally published on May 17, 2020, and updated on January 31, 2021.