Topaz Surgery for Plantar Fasciitis
 When it comes to Plantar Fasciitis, there’s no such thing as a one-size-fits-all treatment plan. And while most podiatrists agree that heel pain can often be treated simply and effectively at home, some cases of complex, stubborn, or chronic Plantar Fasciitis require surgery or medical interventions.
In these cases, making an informed decision with your medical provider and learning all you can about a particular medical procedure can make all the difference in a positive outcome.
Topaz surgery (Topaz MicroDebrider) has recently gained popularity as a minimally invasive medical treatment for chronic and resistant cases of Plantar Fasciitis. But how effective is this new treatment? Are you a good candidate for topaz surgery? What are the possible risks involved? And how much will it cost?
In this post, we’ll cover everything you need to know about the Topaz Procedure:
When it comes to Plantar Fasciitis, there’s no such thing as a one-size-fits-all treatment plan. And while most podiatrists agree that heel pain can often be treated simply and effectively at home, some cases of complex, stubborn, or chronic Plantar Fasciitis require surgery or medical interventions.
In these cases, making an informed decision with your medical provider and learning all you can about a particular medical procedure can make all the difference in a positive outcome.
Topaz surgery (Topaz MicroDebrider) has recently gained popularity as a minimally invasive medical treatment for chronic and resistant cases of Plantar Fasciitis. But how effective is this new treatment? Are you a good candidate for topaz surgery? What are the possible risks involved? And how much will it cost?
In this post, we’ll cover everything you need to know about the Topaz Procedure:
What You Need to Know About Topaz Surgery
While the Topaz Procedure has gotten a lot of attention lately, the procedure isn’t actually new. Topaz has been researched and developed over the past 10 years. Here’s what you should know:What Is Topaz Surgery?
Topaz Surgery, also called Topaz Coblation therapy, is a medical procedure that treats chronic Plantar Fasciitis and Achilles Tendonitis. In the procedure, the doctor uses a special needle-like wand to create two or three dozen small holes, a quarter inch apart, in a grid pattern over the plantar fascia. As the wand enters the skin and fascia, it emits a small burst of radio wave energy, which creates a tiny cut and removes a small amount of tissue. These small cuts help break up scar tissue on the fascia, stimulate a healing response from the body, and increase blood flow and circulation to the injured fascia. The procedure may be performed with either local anesthesia or sedation and takes only 10-20 minutes.How Invasive Is the Topaz Procedure? Does It Hurt?
 One of the best things about Topaz is that, especially compared to fascia release surgery, the procedure is very minimally invasive. The small puncture holes created along the fascia don’t do much damage to healthy tissue, and help reduce trauma to the foot.
Because you will be given either local anesthesia or a light sedative, you should not experience any pain during Topaz, but may feel some pressure as the wand is inserted.
One of the best things about Topaz is that, especially compared to fascia release surgery, the procedure is very minimally invasive. The small puncture holes created along the fascia don’t do much damage to healthy tissue, and help reduce trauma to the foot.
Because you will be given either local anesthesia or a light sedative, you should not experience any pain during Topaz, but may feel some pressure as the wand is inserted.
Is Topaz Covered by Insurance?
Yes, most insurance companies do cover the Topaz procedure for chronic Plantar Fasciitis. If your insurance company covers fascia release surgery, it will likely cover Topaz.How Much Does Topaz Cost?
The cost of Topaz Surgery will vary significantly depending on your insurance coverage, the area where you live, and the type of clinic that performs the surgery. Depending on your insurance coverage, costs may be as little as $500 to as much as $5000.What Is Recovery From Topaz Surgery Like?
Recover from Topaz coblation is generally quicker and easier than fascia release surgery. Typically, patients spend a week following Topaz surgery wearing a walking boot, then normal sneakers with orthotic insoles. After a month to six weeks, most patients report feeling normal again! Compared to plantar fascia surgery, which requires longer downtime and can take two or three months to completely heal, the recovery period after Topaz surgery is relatively brief. Because of the shorter healing period, people with chronic Plantar Fasciitis in both feet sometimes decide to have both feet treated with the Topaz Procedure at once.Is Topaz Surgery Effective for Plantar Fasciitis?
The FDA approved the Topaz Procedure in 2002, and several studies have shown that Topaz is a very effective alternative to fascia release surgery, with about an 80% success rate (similar to plantar fascia release surgery). Be prepared for your pain level to increase immediately following surgery, then get better as your foot heals and you graduate from the walking boot to sneakers and orthotics. Stretching and icing during the healing period can relieve pain and promote recovery, Following your doctor’s post-op treatment instructions is very important for proper healing. Check before deviating from any pain medications prescribed after surgery, for example, and stay consistent in wearing your orthotic inserts even when your foot begins to feel better after surgery. Your healing arch needs support and cushioning now more than ever!Possible Risks of Topaz Surgery
 Like any surgery or medical intervention, the Topaz Procedure has some risk involved. While the following complications are rare, it’s important to talk to your doctor about whether or not they might be significant for your unique situation:
Fascia Rupture: If your plantar fascia has a partial tear (you may not be aware of this), Topaz may put you at risk for Plantar Fascia rupture.
Complications with Other Conditions: If you have certain bone or joint conditions, ligament disorders, neurogenic diseases, or have undergone severe trauma to the foot, Topaz may cause additional complications.
To help reduce these risks and make sure you are a good candidate for Topaz, your doctor may do an MRI or ultrasound of the foot prior to the procedure.
Like any surgery or medical intervention, the Topaz Procedure has some risk involved. While the following complications are rare, it’s important to talk to your doctor about whether or not they might be significant for your unique situation:
Fascia Rupture: If your plantar fascia has a partial tear (you may not be aware of this), Topaz may put you at risk for Plantar Fascia rupture.
Complications with Other Conditions: If you have certain bone or joint conditions, ligament disorders, neurogenic diseases, or have undergone severe trauma to the foot, Topaz may cause additional complications.
To help reduce these risks and make sure you are a good candidate for Topaz, your doctor may do an MRI or ultrasound of the foot prior to the procedure.
Alternatives to Topaz Surgery
If you aren’t a good candidate for Topaz surgery, or you determine that the procedure isn’t the right fit for your situation, the following medical interventions may be good alternatives:Extracorporeal Shockwave Therapy (ESWT):
ESWT is a nonsurgical medical treatment option for Plantar Fasciitis that, similar to Topaz Surgery, uses energy waves to treat the damaged arch. Several studies have shown that it is effective for treating stubborn cases of Plantar Fasciitis; however, it can be somewhat painful, and some insurance companies are reluctant to cover this procedure.Radiation Therapy:
Radiation therapy is another nonsurgical treatment option that may be a good alternative to Topaz, especially for patients with a partial rupture or abnormalities in the foot that might be further complicated by Topaz. Radiation therapy uses small doses of radiation to target the damaged tissue in the fascia. This therapy is effective for about 80% of patients, reasonably priced, has minimal side effects and risks, and is not painful.Intracorporeal Pneumatic Shock Therapy (IPST):
This therapy is similar to ESWT and Topaz, and applies shock waves to heel spurs. Like Topaz, it requires local anesthesia and is minimally painful. A recent study showed a 92% success rate in pain reduction reported by patients.Plantar Fasciitis Surgery:
While fascia release surgery, or plantar fasciitis surgery, is often a last resort because of the downtime, pain, and expense involved, the surgery has a high success rate and may still be a good option for many people with chronic plantar fasciitis. The surgery actually removes part of the damaged plantar fascia and may remove heel spurs as well. Learn more about Plantar Fasciitis Surgery. Topaz surgery shows a great deal of promise as a medical treatment for Plantar Fasciitis; however, the decision of whether or not to undergo this particular procedure will depend on your unique situation. By understanding the potential benefits and risks, learning whether or not you are a good candidate for Topaz, and evaluating how your heel pain has responded to conservative treatment methods, you can make an informed decision with your doctor.Heel Pain During Cancer
 If you’ve been diagnosed with cancer, heel pain and Plantar Fasciitis are likely the furthest thing from your mind.
If you’ve been diagnosed with cancer, heel pain and Plantar Fasciitis are likely the furthest thing from your mind.
However, understanding the unique ways in which cancer may intersect with heel pain–and knowing what to do if heel pain strikes–can help eliminate one more worry and source of pain during an already difficult time.
In this post, we’ll discuss how cancer treatments can contribute to Plantar fasciitis, special considerations for treating heel pain alongside cancer, and whether or not heel pain itself can be an indicator of cancer.
Can Heel Pain Be a Side Effect of Cancer Treatments?
Cancer treatments come with a host of unpleasant, painful, and confusing side effects–as if cancer itself isn’t difficult enough!
Not only can chemotherapy, radiation, and various oral medications cause nausea, extreme tiredness, and hair loss–but they can also contribute directly or indirectly to Plantar Fasciitis and heel pain.
Many of these cancer treatments contribute to loss of bone density and muscle wasting. Both of these side-effects can have a big impact on the arch’s ability to properly absorb the impact from even simple activities like walking. As treatments continue, the arch may flatten and become more susceptible to small tears, stress, and micro injuries. This condition, known as Plantar Fasciitis, can result in mild to severe heel pain.
And while some cancer treatments result in weight loss and drastically reduced appetite (such as chemotherapy), other oral medications can cause rapid weight gain or bloating. This sudden weight gain places a lot of extra strain on the arch of the foot, causing it to flatten and sustain damage.
Treating and Preventing Heel Pain Alongside Cancer
Most cases of heel pain can be treated without costly or invasive medical treatments. Which is good news if you have cancer, since costly and invasive medical treatments are the name of the game.
An incredible 90% of Plantar Fasciitis cases can be resolved without surgery, using treatments including the following:
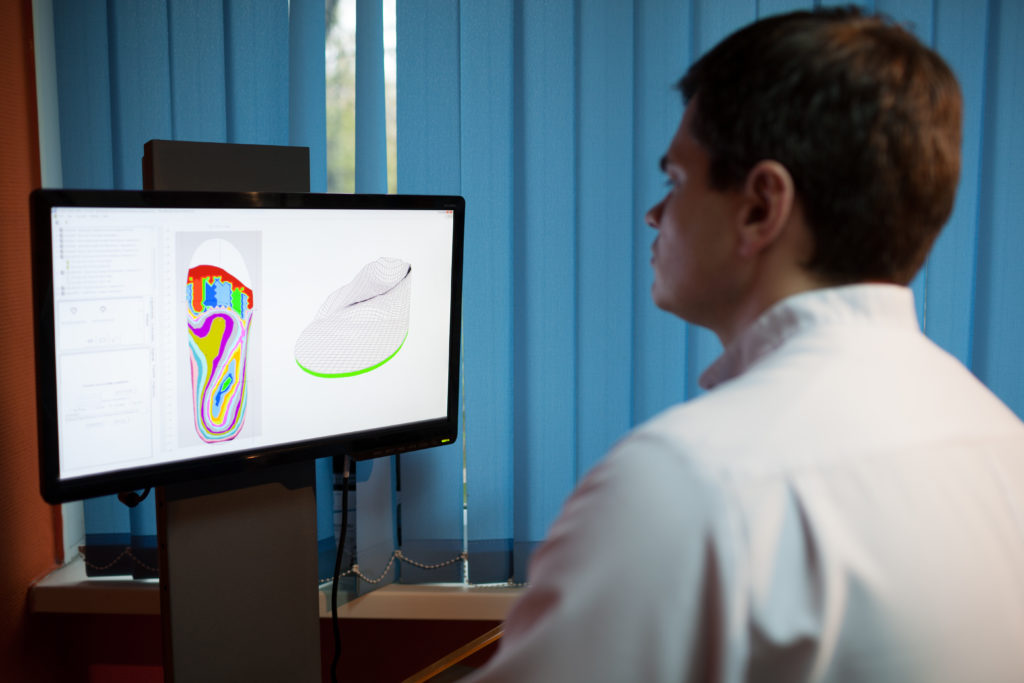
Orthotics: Orthotic inserts designed to target Plantar Fasciitis (not just the foam grocery store inserts), are one of the best ways to treat heel pain symptoms while actually addressing the root of the problem–a damaged and unsupported arch. These special inserts, called Heel Seats, apply targeted acupressure to relieve pain, lift the arch to an optimal height, provide durable (and washable!) cushioning, and provide the backup your arch needs–all for the cost of a few cups of coffee.
Stretching: Gentle stretches for the heel, ankles, toes, and calves, can have a big impact on your arch’s elasticity and ability to bear weight properly. Many stretches can be done from bed while you rest, for just a few minutes a day. Stretching can also promote improved blood flow and a boost in endorphins, which may be sorely needed during difficult cancer treatment regimens.
Night Splints or Socks: During exhausting cancer treatments, even stretching in bed can be too much effort. Using a night splint (or a sock night splint for extra comfort and softness), you can hold your foot in a gentle stretch all night long, significantly improving the pain from Plantar Fasciitis–especially those first few steps out of bed.
Icing and Self Massage: Simple pain-relief techniques like icing and self massage (with either your fingers or a variety of household items), can make a big difference in your heel pain. Use icing and massage as often as you need throughout the day, spending 10-20 minutes on the injured area.
When Is Heel Pain an Indicator of Cancer?
The vast majority of cases involving heel pain are diagnosed as Plantar Fasciitis or other non-cancerous conditions. However, chronic heel pain can be an indicator of cancer in rare cases. Studies have documented cases in which lung cancer or breast cancer presented as s metastasized lesion on the heel bone, which was initially diagnosed as plantar fasciitis. Other forms of cancer that attack the blood, bones, and lymph nodes may present anywhere in the body and may, at times, show up in the foot or heel.
If you notice unusual (but typically painless) lumps or hard bumps on the feet or heels, there’s no need to immediately assume a diagnosis of cancer, however. Most bumps and lumps are benign and a result of shoes rubbing or irritating the tissues of the foot (including Haglund’s Deformity (pump bump), retrocalcaneal bursitis, and cysts). However, if you notice symptoms like fatigue, swollen lymph nodes, fever, or unexplained weight loss in addition to your heel pain or lump on the foot, it’s important to make an appointment with your doctor. It’s also a good idea to see a doctor for heel pain or bumps on the heel or foot that don’t seem to respond to conservative remedies or seem to be growing.
Remember: In the vast majority of cases, heel pain is an unfortunate side effect of some cancer treatments–not an indicator of the presence of cancer. However, in either case, knowledge is key to healing and your health.
If you’re currently undergoing (or have recently undergone) cancer treatments, and now struggle with heel pain, take comfort in knowing that your heel pain doesn’t have to be one more worry on your mind. With simple, inexpensive home treatment options such as orthotic inserts, stretching, a night splint, and icing and massage techniques, most people can simply and effectively address the condition at home.
5 Tricks for When You Can’t Sleep from Nighttime Heel Pain
 Plantar Fasciitis is often associated with excruciating morning pain in the form of shooting or stabbing sensations that accompany those first steps out of bed each day.
Plantar Fasciitis is often associated with excruciating morning pain in the form of shooting or stabbing sensations that accompany those first steps out of bed each day.
But many people who suffer from Plantar Fasciitis also experience heel pain in the middle of the night, which can make for a long, sleepless, and painful night.
What can you do if you wake up in the middle of the night with painful heels? These five tricks will help you get back to sleep–and back to healthy arches–in no time.
Trick #1: Keep a Ball on Your Nightstand
A quick massage using items you probably already have at home can provide effective, simple pain relief in the middle of the night. Keep a tennis ball, golf ball, (or a washable Foot Massage Ball) on your nightstand. If heel pain from Plantar Fasciitis wakes you up in the week hours of the night, simply swing your leg over the edge of the bed and spend a few minutes applying gentle but firm pressure as you roll the ball along the floor from your heel to the ball of your foot, along the arch. This gentle massage will increase blood flow, disrupt pain signals in the nerves, and break up adhesions and scar tissue along the plantar fascia.
Keep the massage going for approximately sixty seconds, then take a break and repeat once more, honing in on any “hot spots” you find that are extra painful. To avoid waking up more than necessary, keep your eyes closed and the lights off in your room while you perform this massage.
Trick #2: Try Ice Slippers
Icing is a tried and true method for temporary pain relief. But by the time you find a baggie, fill it with ice, and hold it in the right spot for 20 minutes, you’re likely to be wide awake. And the last thing you need is pain relief that disrupts your sleep even more.
Thankfully, an innovative and inexpensive product can help: Ice Therapy Slippers are foot-shaped ice packs that can be strapped right onto the bottom of your foot. No mess, no fuss, and you can fall back asleep quickly without fear of waking up in a puddle!
Trick #3: Sleep with a Night Splint or Sock Splint
If you find yourself waking up with night pain from Plantar Fasciitis regularly, it may be possible to head off the problem completely by wearing a night splint or soft night splint while you sleep. Both products hold the foot or feet in a gentle stretch all night long, avoiding the tightness and stiffness associated with a damaged arch.
Choose a night splint that is durable, lightweight, and breathable enough that it won’t disrupt your sleep (you’ve had enough of that!). Or, if you’re looking for a softer, lighter alternative, choose Plantar FXT night splint for maximum comfort. Night splints have the added benefit of reducing morning pain that accompanies Plantar Fasciitis, in addition to helping relieve night pain.
Trick #4 Stretch in Bed
The idea of stretching in the middle of the night might sound unappealing–and a fast way to completely wake yourself up. But several effective stretches can be performed in bed, with the lights off, using just a pillowcase or a hand towel. This series of stretches can help loosen tight ligaments in the foot and calves, improve circulation to the nerves and tissue, and relieve the pain that woke you up in the first place:
Simply sit up in bed, keeping your legs together and your feet extended. Keep your eyes closed, and stay relaxed and calm while you slowly point your toes outward and down, ten times.
Next, wrap that pillowcase or hand towel around the ball of one foot, keeping hold of both ends. Sit up straight, and use your arms to gently but firmly pull the ball of your foot back toward your body, while you flex the foot. Hold the stretch for thirty seconds (letting your arms do the pulling, not the flex of your foot), then switch to the other foot.
Finish this series of stretches in bed with a short massage of the arches and calves, using your fingers and thumbs.
Trick #5 Elevate Your Legs and Feet
Use a pillow to elevate you feet slightly while you sleep, to improve blood circulation and reduce swelling and inflammation from Plantar Fasciitis. Feet can be safely elevated at six to twelve inches while you sleep, using a standard pillow. Or, if you’re a side sleeper, you may find a body pillow to be more comfortable in elevating just the affected foot while you sleep on your side and hug the pillow to your body.
Waking up in the middle of the night is a bothersome experience all by itself. Add heel pain to the mix, and it’s a dark night indeed. However, by using these simple tricks (and by committing to a dedicated routine of Plantar Fasciitis treatments during the day!), you can get back to dreamland quickly!
Heel Pain Without Trauma or Injury
 While heel pain and Plantar Fasciitis can be the direct result of sports injuries or foot trauma, it’s also common for these conditions to develop in the absence of a dramatic or sudden impetus.
While heel pain and Plantar Fasciitis can be the direct result of sports injuries or foot trauma, it’s also common for these conditions to develop in the absence of a dramatic or sudden impetus.
In fact, heel pain that onsets gradually can be even more insidious–since it may be mild at first, and easier to brush off as insignificant. However, if the factors causing your heel pain persists over time, you may be setting yourself up for a long road to recovery, or even long-term damage.
In the blog post, we’ll explore some of the most common causes of heel pain that develops seemingly out of the blue. We’ll also cover conservative treatment options that have been proven to both treat and prevent heel pain:
Plantar Fasciitis Without Injury
While Plantar Fasciitis isn’t the only reason that heel pain may develop in the absence of trauma or injury, it’s certainly the most common. The American Academy of Family Physicians lists Plantar Fasciitis as the number one cause of heel pain and estimates that more than 2 million people seek treatment for the condition each year.
Plantar Fasciitis that develops gradually over time is typically caused by the following factors:
Obesity or Rapid Weight Gain:
The arch of the foot exists to absorb and distribute the impact from running, walking, and jumping. However, with excess weight comes an additional burden to the arch. Pregnancy or rapid weight gain can cause damage and cumulative strain to an unsupported arch.
The Aging Process:

As we get older, our arches naturally decrease in flexibility and strength, making them more susceptible to small tears, flattening, strain, and degeneration.
Excessive Pronation or Underpronation:
Irregularities in gait, such as underpronation or pronation (conditions that cause of the foot to roll outward or inward while you walk), can damage or strain the arch of the foot over time.
Ill-Fitting or Unsupportive Footwear:
Your shoes can make a big difference in how your arch absorbs and distributes impact. Footwear that doesn’t fit properly or support and cushion your arch can lead to Plantar Fasciitis over time.
Work Conditions or Exercise Regimens:
Whether you’re on your feet, walking, or running a lot for work or exercise, this wear and tear can have a cumulative effect in straining or breaking down your arch unless it is properly cushioned and supported.
Other Causes of Heel Pain Without Trauma
Numerous conditions that cause heel pain can develop in the absence of trauma or injury. Most of these conditions develop gradually over time, due to unsupportive or worn footwear, carrying extra weight that places strain on the heel and arch, or simply wear and tear from overuse.
Bursitis of the Heel:
Bursitis develops when the retrocalcaneal bursa, or the fluid-filled sacs that cushion and lubricate the back of the heel, become inflamed and irritated through rubbing or pressure over time. Bursitis results in pain at the back of the heel (where the heel meets the Achilles tendon), inflammation, redness, and tenderness.
Learn More About Bursitis of the Heel.
Tarsal Tunnel Syndrome:
Tarsal Tunnel Syndrome is similar to carpal tunnel syndrome–except the condition develops in the feet. When the tibial nerve is pinched or obstructed over time, the amount of blood flow to this nerve decreases and results in pain and inflammation. The condition often develops in tandem with arthritis, obesity, or heel spurs.
Learn More About Tarsal Tunnel Syndrome.
Haglund’s Deformity:

This condition is also known as “pump bump,” and causes a painful lump to form on the back of the heel. Haglund’s Deformity is usually caused by prolonged use of unsupportive shoes like high heels.
Learn More About Haglund’s Deformity.
Posterior Tibial Tendonitis:
If your heel pain is primarily located on the inside of the foot, ankle, shin, or heel, you may have posterior tibial tendonitis. The condition develops over time in response to overuse and irritation of the posterior tibial tendon. You may have this condition if standing on one foot while trying to lift your heel off the ground is extremely painful.
Learn More About Posterior Tibial Tendonitis.
Treating Heel Pain and Plantar Fasciitis
Whether your heel pain is related to Plantar Fasciitis, posterior tibial tendonitis, or Haglund’s Deformity, the most important steps you can take toward healing are identifying the causes of your pain (for example, ill-fitting or unsupportive footwear), then taking consistent and proactive steps to relieve your pain and promote healing.
While chronic or severe heel pain that does not respond to conservative treatments may require more invasive or expensive medical interventions, most cases of heel pain–particularly cases of Plantar Fasciitis–can be treated successfully and inexpensively at home:
Icing
To reduce redness, inflammation, pain, or swelling, apply an ice pack for twenty minutes, two or three times each day.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
NSAIDs like Ibuprofen can reduce swelling and pain, making you more comfortable while you recover and rest.
Rest
The importance of rest can’t be overstated, particularly if your heel pain is being caused by overuse. Set a schedule of rest breaks several times a day, sitting or lying down, taking the pressure off your heel and arch. Rest will help facilitate the healing of Plantar Fascia of micro-injuries and allow the arch to “bounce back” over time.
Stretching
Simple stretches, performed once or twice a day for 10-15 minutes can improve the strength and flexibility of the Plantar Fascia ligament and surrounding muscles and tissue. A strong, flexible arch is an arch that can withstand greater impact and weight!
Replace or Retire Your Worn or Unsupportive Footwear
Those red high heels might be snazzy, but they aren’t worth long-term pain and damage to the arch of your foot. Reserve unsupportive footwear for infrequent, short-term activities, replace worn shoes, and fortify your flats with additional arch support in the form of orthotic inserts.
Orthotic Support
Orthotic inserts such as Heel Seats were made especially for Plantar Fasciitis. These inserts can add additional arch support and cushioning to almost any pair of shoes, and lift the arch to an optimal level for absorbing impact and distributing weight.
Remember, while your heel pain has seemingly appeared suddenly and mysteriously, the cause has likely been brewing for some time as a result of weight gain, an unbalanced gait, improper footwear, or a weak arch. Keep this fact in mind as you approach conservative treatment options like icing, stretching, orthotics, and rest. These remedies won’t fix the problem overnight. However, with patience, consistency, and time, more than 90 percent of plantar fasciitis cases can be resolved successfully without medical intervention.
Plantar Fasciitis in One Foot
While your feet work in tandem to walk, run, and jump, they don’t always experience injury or trauma in the same way.
Suffering from heel pain or Plantar Fasciitis in just one foot is common. However, this unbalanced condition raises plenty of questions about why Plantar Fasciitis developed this way, and how to involve the unaffected foot in your treatment regimen.
Keep reading to learn what to do when you have heel pain in just one foot:
Why Plantar Fasciitis May Develop in Just One Foot
Plantar fasciitis may develop in just one foot under a variety of circumstances.
Injury or Trauma
Injury or trauma that affects just one foot (for instance, a car accident, sprain, or fall) is one of the more obvious reasons that Plantar Fasciitis may develop in one foot, since the arch and heel may be injured or damaged. However, just as often Plantar Fasciitis and heel pain develops in the uninjured foot, which may be forced to absorb greater impact and force to compensate for the injured foot. It’s also important to note that it’s also common for heel pain to develop without any sort of injury.
Surgery (Including Plantar Fasciitis Surgery!)
The healing period (usually around six weeks) following a broken bone (including bones in the leg) or foot surgery like a bunionectomy or plantar fascia release requires plenty of rest for the affected area. Like the previous scenario, this can place a great deal of additional strain on the healthy foot, particularly if there is already an abnormality in gait or arch height.
Imbalanced Gait
Subtle differences in arch height, foot structure, and muscle tightness can mean that your feet experience impact differently while you walk, run, or jump. Over time, the heavier wear and tear on one foot can lead to expedited arch trauma and breakdown in that foot.
Overlapping Foot Conditions
Bunions, hammer toe, cysts, or Morton’s Neuroma in one foot can lead to Plantar Fasciitis in either the affected or unaffected foot, depending on how this overlapping foot condition interacts with your gait and your arches’ ability to bear impact.
Special Considerations for Treating Heel Pain in One Foot

Most proven, tried-and-true conservative treatment methods for Plantar Fasciitis are geared toward both feet. However, with a few tweaks, these at-home treatments can be just as effective for one foot. The most important question to answer is whether both feet (or just the affected foot) should be treated:
Orthotics: Both Shoes or Just One?
Orthotic inserts should be worn in both shoes–not just one. Not only will wearing a complete set of orthotics avoid gait imbalances, but it will prevent another imbalance in strain and impact on your healthy foot from developing. Orthotics add an extra layer of cushioning, support, and targeted acupressure that is beneficial for all feet.
Click here to get 100% guaranteed orthotic inserts.
Night Splints: Both Feet or Just One?
There’s no need to use a night splint or Sock Splint for both feet–just the affected foot. Night splints head off morning pain by keeping the damaged plantar fascia ligament in a gentle, flexed stretch all night long to stimulate blood circulation and keep the ligament flexible.
Stretching and Massage: Both Feet or Just One?
Stretching is one of the best ways to improve the strength and flexibility of a damaged plantar fascia, as well as the surrounding muscles and ligaments that support the arch of the foot. It’s important to stretch both sets of heels, calves, and ankles to ensure that both feet and legs are at max capacity to resist injury and bear weight and impact.
Rest: Both Feet or Just One?
It’s important to give both feet regular rest periods, even if only one foot has symptoms of Plantar Fasciitis. Your natural inclination will be to favor the injured foot or rest it more frequently–which can lead to the development of symptoms in the healthy foot as it absorbs extra stress and impact. Take regular breaks from standing or walking to rest both feet and allow your body to heal and recover.
Whether you have Plantar Fasciitis in both feet or just one, the most important thing you can do is take your symptoms seriously and start a treatment regimen as soon as possible. With early intervention, a dedicated routine of proven home-healing techniques, and a little patience, most cases of Plantar Fasciitis can be resolved easily and successfully.